Storing medications safely in a shared living space isn’t just about keeping pills out of reach-it’s about preventing accidents, protecting effectiveness, and avoiding legal or health risks. Whether you’re living with aging parents, adult children, roommates, or in a group home, improper storage can lead to accidental overdoses, spoiled drugs, or even misuse. The good news? With a few practical steps, you can make medication storage simple, safe, and stress-free-even in crowded homes.
Why Medication Storage in Shared Spaces Is Different
In a single-person home, you might toss pills in a bathroom cabinet or leave them on the nightstand. But in shared spaces, that’s a recipe for trouble. Children might find grandma’s painkillers. Someone with a substance use disorder could take a neighbor’s prescription. Or worse-medications get exposed to heat, humidity, or temperature swings that ruin them. According to a 2025 survey by SeniorHelpers, 67% of multi-generational households had at least one medication-related incident in the past year. Over 40% of those cases involved kids grabbing pills from bathroom cabinets. Meanwhile, insulin and other temperature-sensitive drugs lost potency when stored on refrigerator door shelves, where temperatures can swing by 10°F or more. The solution isn’t complicated, but it does require structure. You need to treat medications like valuables-because they are.Step 1: Remove Expired and Unneeded Medications
Before you set up a storage system, clean house. Go through every medicine cabinet, drawer, and fridge. Check expiration dates. Look for pills that are discolored, cracked, or smell odd. If someone moved out or passed away, their meds shouldn’t stay. The FDA says most medications lose effectiveness after their expiration date-but some, like insulin or liquid antibiotics, can become dangerous. Don’t flush them or toss them in the trash. Take them to a local pharmacy drop-off or a community take-back event. In Ireland, you can return unused meds to any pharmacy for safe disposal-no questions asked. Only keep what’s actively being used. A cluttered medicine drawer makes it harder to track what’s real and what’s old.Step 2: Categorize by Storage Needs
Not all medications need the same conditions. Group them by how they must be stored:- Refrigerated: Insulin, some eye drops, certain antibiotics, and biologics. Must stay between 36°F and 46°F (2°C-8°C). Store in the center of the fridge, not the door.
- Room temperature: Most pills, tablets, and capsules. Keep away from heat and moisture-so not the bathroom or near the stove.
- Controlled substances: Opioids, benzodiazepines, ADHD meds. These require locked storage and are legally restricted.
Step 3: Choose the Right Storage Location
The best place for meds isn’t the bathroom. It’s not the kitchen counter. It’s not under the sink. For shared homes, the safest option is a locked drawer or cabinet in a bedroom-preferably one that belongs to the person taking the meds, or a central location with limited access. A simple key-lock drawer from a hardware store works fine. No need for high-tech safes unless you’re storing controlled substances. In professional care homes, 100% of large facilities have dedicated medication rooms. But in family homes, only 28% use locked storage. That gap is dangerous. If you have kids, teens, or visitors, a locked drawer is non-negotiable. If someone needs refrigerated meds, use a small, dedicated mini-fridge if possible. If not, clearly label the fridge shelf with the person’s name and use a lockable container inside. Never mix food and meds in the same drawer or container.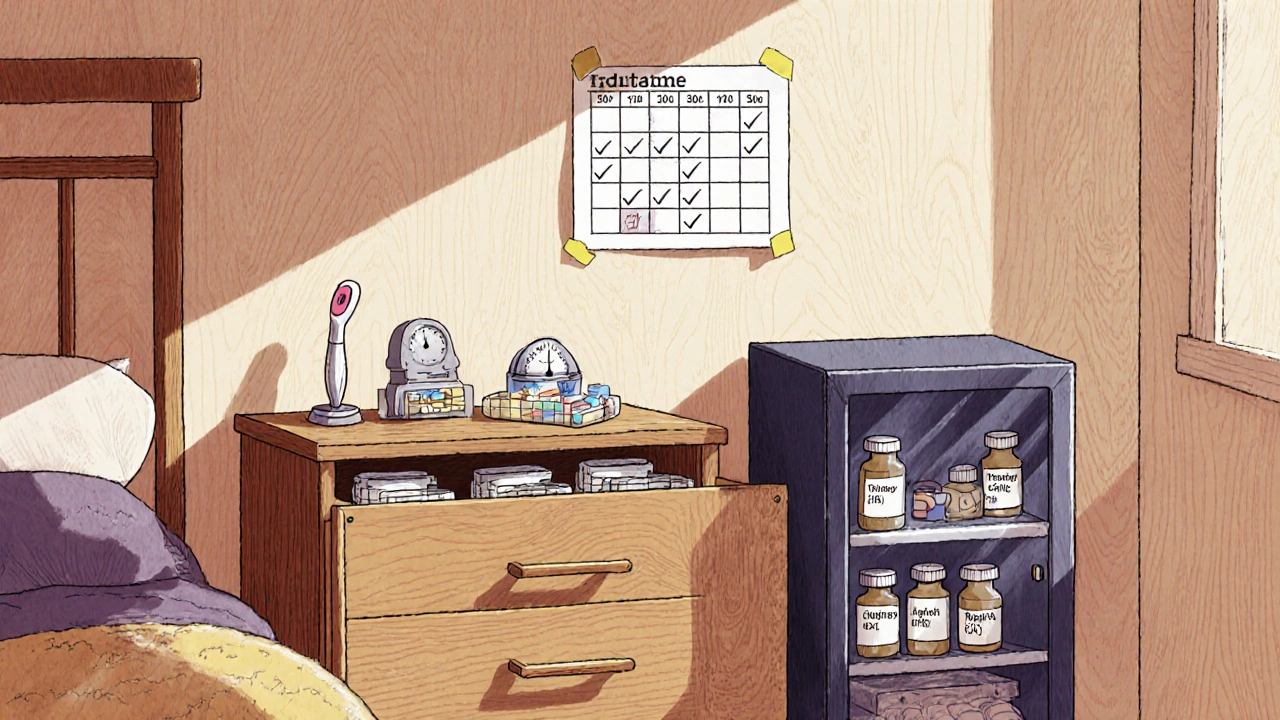
Step 4: Lock It Down-Especially for Controlled Substances
If someone in the home takes opioids, stimulants, or anti-anxiety meds, federal and state laws require those to be stored in a locked container, accessible only to authorized users. In Ireland, the HSE guidelines treat these as high-risk items-unauthorized access can lead to legal consequences. Use a lockbox with a combination or key. Some models even have digital logs that record who opened it and when. These cost under €50 and are worth every euro if they prevent misuse. Don’t assume someone “wouldn’t take it.” People do-especially under stress, in pain, or during a crisis. Locking it isn’t distrust-it’s responsibility.Step 5: Label Everything Clearly
A pill bottle labeled “John” isn’t enough. What if John’s son takes it thinking it’s his own? Or a visitor grabs it because it looks like a headache pill? Each container should have:- The person’s full name
- The medication name (both brand and generic)
- Dosage and frequency
- Expiration date
Step 6: Document the Schedule
In care homes, staff use Medication Administration Records (MARs) to track who took what and when. You don’t need fancy software-but you do need a simple system. Create a printed chart with:- Names of everyone taking meds
- Medication names
- Time and dose
- Box to check off after each dose
Step 7: Train Everyone Who Might Access It
Kids, teens, visiting relatives-they all need to know this isn’t candy. Have a short family meeting. Say it plainly: “These aren’t snacks. Taking someone else’s pills can make you sick-or worse.” If you have a teen with ADHD who takes stimulants, explain why their meds are locked. If your partner has diabetes, show them how to check the fridge shelf. Make it normal, not secretive. Some families use a “medication buddy” system-where one person is responsible for checking the schedule and refills each week. That reduces confusion and builds accountability.
Step 8: Monitor Temperature and Environment
Heat and moisture destroy meds faster than you think. A study from Johns Hopkins found that some antibiotics lose up to 30% of their strength in just 24 hours if stored in a hot bathroom. Keep all meds:- Away from direct sunlight
- Off the floor (dust, spills)
- Not near sinks, showers, or stoves
- In a cool, dry place (like a bedroom dresser)
What to Do If Something Goes Wrong
Accidents happen. A child swallows a pill. Someone takes the wrong dose. A fridge breaks. Here’s what to do immediately:- Call emergency services or your local poison control center (in Ireland, call 1800 222 444).
- Don’t wait for symptoms. Even if the person seems fine, get help.
- Keep the pill bottle or packaging-you’ll need the info.
- Afterward, review your storage system. What broke? How can you fix it?
Tools That Help
You don’t need fancy gadgets, but some tools make life easier:- Lockable pill organizer: Holds daily doses and locks shut. Great for people who take multiple meds.
- Mini-fridge with lock: Under €100. Perfect for insulin or eye drops.
- Smart lockbox: Logs access, tracks temp. Brands like DosePacker now offer these for home use.
- Medication reminder app: Syncs with the printed chart. Useful if someone lives remotely but helps manage care.
Final Thought: It’s About Respect, Not Control
Locking up meds isn’t about spying on people. It’s about protecting them-from themselves, from accidents, from harm. In shared spaces, everyone’s health is connected. One person’s mistake can affect the whole household. By setting up clear, simple, secure systems, you’re not just storing pills-you’re building trust. Start small. Clean out the cabinet. Lock one drawer. Label one bottle. Do one thing today. The rest will follow.Can I store all medications in the same locked drawer?
Yes, as long as they’re all room-temperature medications. But refrigerated items like insulin must be kept cold. Store those in a separate locked container inside the fridge. Controlled substances like opioids should always be in their own locked box, even if other meds are in the same drawer.
Is it okay to keep meds in the bathroom?
No. Bathrooms are too humid and hot, especially after showers. Moisture can break down pills, and temperature swings reduce effectiveness. Plus, it’s the most common place kids find pills. Store meds in a dry, cool bedroom drawer instead.
What if someone refuses to lock their meds?
Talk to them calmly. Explain that it’s not about distrust-it’s about safety. If they’re worried about losing access, offer to help them carry a small daily pill organizer with their current doses. Many people agree once they realize how common accidents are.
How do I know if a medication has gone bad?
Look for changes: pills that are cracked, discolored, or smell odd. Liquid meds that are cloudy, thick, or have particles. If you’re unsure, call your pharmacist. Never guess-especially with insulin, antibiotics, or heart meds.
Can I use a regular pill organizer for everyone?
Only if each person has their own labeled organizer. Never mix meds in the same container-even if they look alike. A pill organizer meant for one person can become a hazard if others use it. Use color-coded or name-labeled boxes to avoid confusion.
What should I do with old or unused meds?
Return them to any pharmacy in Ireland-they’re required to take them back for safe disposal. Don’t flush them, burn them, or throw them in the trash. Pharmacies have special bins for this. It’s free, legal, and protects the environment.
Do I need to track every dose if I live with a roommate?
If you’re not responsible for administering their meds, no. But if you’re helping someone manage their schedule-like an elderly parent or a sibling with a chronic illness-then yes. A simple checklist on the fridge helps prevent missed doses and double-dosing. It’s not bureaucracy-it’s care.


David Cunningham
Just moved into a shared house with my sister and our mom. We did the locked drawer thing last week and honestly? Life’s way calmer now. No more midnight pill hunts or weird smells from expired antibiotics. Also bought a mini-fridge for her insulin-€60 on Amazon, worth every cent.
Rahul Kanakarajan
Lmao this is so overkill. People used to just keep pills in the bathroom and lived fine. Now we need lockboxes and temperature logs? My grandma took her blood pressure meds out of a sock drawer for 40 years and never died. Stop treating adults like toddlers.
Justin Daniel
Bro, I get the sarcasm, but Rahul… you’re literally describing the reason we need these systems. I had a cousin take a stranger’s Xanax at a party because it looked like his own. He ended up in the ER. It’s not about distrust-it’s about dumb luck running out. The bathroom thing? That’s not tradition, that’s negligence.
New Yorkers
Ah yes, the modern American obsession with control disguised as care. We’ve turned medicine into a sacred relic guarded by paranoid priests with lockboxes and spreadsheets. What happened to trust? What happened to personal responsibility? We are not children. We are not cattle. We are humans-flawed, messy, and beautifully imperfect.
Melvina Zelee
i mean… i get the drama but also? i think its kinda beautiful that we’re finally starting to treat health like something that matters. not just ‘oh this pill’s here, someone’ll take it’-but like, no, this is someone’s life. and if we’re living together, we’re kinda responsible for each other’s safety. even if it’s awkward. even if it’s extra. even if it feels like micromanaging. we’re all just trying not to die accidentally, right?
james lucas
so i did the clean out thing last month and holy crap i found 3 different kinds of ibuprofen from 2019, a bottle of my ex’s antidepressants (why??), and a half-used tube of eye drops that looked like it had been through a war. i threw it all out and got a cheap lockbox from walmart for like $15. now my roommate doesn’t freak out when he sees my ADHD meds. we even made a little chart on the fridge with names and times. it’s weirdly satisfying??
Jessica Correa
My mom has diabetes and I help her manage her meds. We use a pill organizer with her name on it and keep it locked in her nightstand. The chart on the fridge? We just use a dry erase board. I write ‘AM’ and ‘PM’ and check it off. Simple. No app needed. And yes, we still have the insulin in the fridge center shelf. No door. Ever.
Michael Fitzpatrick
Just wanted to say this article saved my sanity. My brother has chronic pain and takes opioids. He was so defensive about locking them up-said I didn’t trust him. But when I showed him the stats about teens grabbing meds from bathroom cabinets? He paused. Then he said, ‘You know what? I don’t want anyone else’s kid to have to go through what I went through.’ We got a smart lockbox. It even texts me if someone opens it. He says it’s weirdly comforting. Who knew?
ann smith
This is so important ❤️ I work in home care and see way too many cases where meds are just… left out. One lady had her blood thinner next to her coffee maker. One day her grandson thought it was sugar. He put it in his oatmeal. We got lucky he didn’t bleed out. Please, please, please-lock it. Label it. Don’t wait for a tragedy to act. You’re not being overprotective-you’re being loving.
Julie Pulvino
My roommate and I have a shared fridge. We put all our meds in a small plastic bin with a lid and labeled it ‘MEDS ONLY-NO FOOD’. It’s not locked but we have an unspoken rule: don’t touch. Works fine. Also, we take turns checking expiration dates every month. It’s become this weird little ritual. Kinda nice, honestly.
Patrick Marsh
Locked drawer. Yes. Refrigerated meds? Separate. Controlled substances? Locked box. Labeling? Mandatory. Temperature? Monitor. Schedule? Track. Training? Required. No exceptions. This isn’t optional. This is basic hygiene for shared living. If you’re not doing this, you’re gambling with lives.
Danny Nicholls
just got one of those smart lockboxes with the temp sensor and i’m obsessed 😍 it’s like having a nurse in my drawer. also bought a mini fridge with a lock for my insulin. now my roomie thinks i’m a wizard. i just say ‘it’s called responsibility’ and he nods. we even made a little sign: ‘meds = love, not snacks’ 🤓❤️
Shawn Daughhetee
my dad passed last year and we found like 12 bottles of his meds still sitting in the cabinet. some were expired. some were for different people. i cried cleaning them out. now i keep everything locked and labeled. i dont want anyone else to have to do that. it’s not about control. it’s about not letting grief turn into more pain
Robin Johnson
Look. I get that some of this feels excessive. But here’s the thing: if you wouldn’t leave your car keys on the counter for a 14-year-old to grab, why would you leave your prescription opioids there? It’s not paranoia. It’s basic risk management. Start with one step. Lock one drawer. That’s your win. Do it today.
luke young
My niece is 8 and she thinks my anxiety pills are candy. I used to keep them on my nightstand. Now they’re locked in a drawer she can’t reach. She asked me why. I told her, ‘Because these aren’t candy-they’re medicine, and medicine is serious.’ She nodded like she understood. I hope she does.