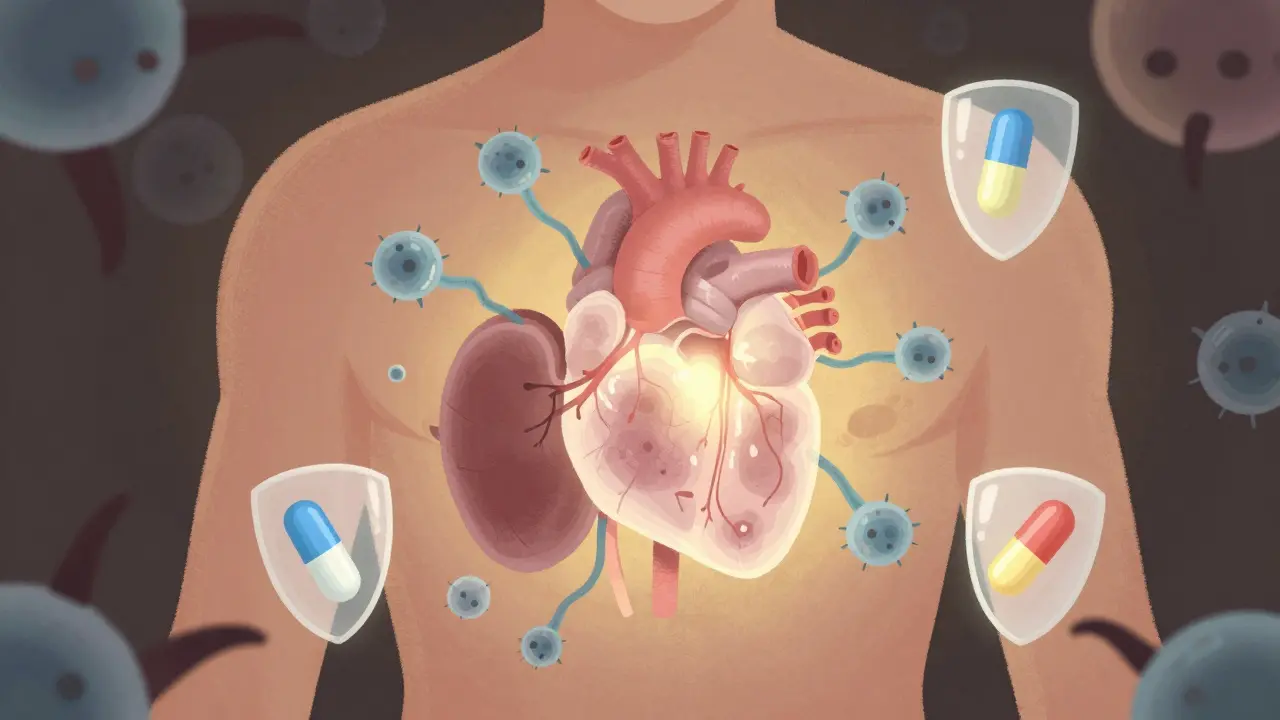
After a transplant, your body doesn’t know the new organ belongs to you. It sees it as an invader. That’s why you need immunosuppressants-medications that quietly turn down your immune system so your kidney, heart, liver, or lung isn’t attacked and destroyed. But here’s the catch: lowering your defenses doesn’t just protect the transplant. It leaves you wide open to infections, cancers, and serious side effects. Getting this balance right isn’t optional. It’s life-or-death.
Why Immunosuppressants Are Non-Negotiable
Without these drugs, most transplants fail within weeks. In the 1950s, before cyclosporine was developed, up to 80% of kidney transplants were rejected. Today, thanks to modern immunosuppressants, that number has dropped to under 15%. That’s a massive win. But survival isn’t just about avoiding rejection. It’s about living well long after surgery.These medications don’t just prevent rejection-they extend life. Transplant recipients live longer and feel better than people on dialysis or waiting for another organ. But the trade-off is real. Your immune system is suppressed. Not just for months. For the rest of your life.
The Four Main Classes of Immunosuppressants
There’s no single drug that does it all. Doctors use combinations, each targeting a different part of the immune system. Here’s what you’re likely taking:- Calcineurin inhibitors (cyclosporine, tacrolimus): These are the backbone of most regimens. They stop T-cells from sounding the alarm. But they’re hard on the kidneys. About 30-50% of long-term users develop chronic kidney damage from them. They also raise blood pressure, cause tremors, and spike blood sugar.
- Corticosteroids (prednisone): Powerful but brutal. Used early after transplant to calm inflammation, they’re often tapered down. Still, even low doses can cause diabetes in up to 40% of patients, thin bones (osteoporosis) in half of long-term users, and weight gain that’s hard to lose.
- Antiproliferatives (mycophenolate mofetil, azathioprine): These block immune cells from multiplying. Mycophenolate is common now because it’s less toxic than azathioprine. But it causes nausea, vomiting, and diarrhea in up to half of users. It can also drop your white blood cell count, making infections more likely.
- mTOR inhibitors (sirolimus, everolimus): These are alternatives for people who can’t tolerate calcineurin inhibitors. They’re gentler on the kidneys but come with their own risks: delayed wound healing, serious lung inflammation (pneumonitis), and high cholesterol. Everolimus carries a black box warning for kidney clotting in the first 30 days after transplant.
Doctors mix and match these based on your organ, age, other health problems, and how your body responds. A liver transplant patient might avoid sirolimus entirely because it’s linked to higher death rates in that group. A kidney patient might switch from cyclosporine to tacrolimus if their kidneys start to decline.
The Hidden Dangers: Infections and Cancer
Your immune system doesn’t just fight off viruses. It hunts down cancer cells before they grow. When you suppress it, that protection vanishes.Transplant patients have a 2 to 4 times higher risk of developing cancer than the general population. Skin cancer is the most common-especially squamous cell carcinoma. That’s why yearly full-body skin checks are mandatory. Other cancers linked to immunosuppression include lymphoma, Kaposi sarcoma, and cervical cancer.
Infections are just as dangerous. You’re not just at risk for colds and flu. You’re vulnerable to rare, deadly bugs like cytomegalovirus (CMV), which can cause pneumonia or organ damage. Fungal infections like aspergillosis and bacterial infections like listeria are also serious threats.
That’s why most patients get antiviral, antifungal, and antibiotic prophylaxis for the first 3 to 6 months after transplant. Even after that, you need to be extra careful. Wash your hands. Wear a mask in crowded places. Avoid gardening or cleaning bird cages. Skip raw sushi and undercooked meat. These aren’t suggestions-they’re survival rules.
Adherence: The #1 Cause of Transplant Failure
You can have the perfect drug combo, the best doctor, the cleanest lifestyle-but if you miss a dose, it all falls apart.Studies show that more than half of kidney transplant patients don’t take their meds exactly as prescribed. Some forget. Some skip doses because they feel fine. Others can’t afford the pills. One missed dose might not cause immediate rejection. But over time, it adds up. Nonadherence increases the risk of acute rejection by nearly three times. For heart transplant patients, it raises the chance of transplant coronary artery disease by 3.5 times.
Complex regimens make it worse. Taking five pills at three different times a day is a nightmare. That’s why many clinics now switch patients to once-daily versions of tacrolimus or mycophenolate. Simple changes like pill organizers, phone alarms, and apps that send reminders can boost adherence by 15-25%.
Monitoring: Blood Tests Are Your Lifeline
You can’t feel when your tacrolimus level is too high or too low. That’s why blood tests are non-negotiable.Too much immunosuppressant? You risk kidney damage, nerve problems, or even seizures. Too little? Your body starts attacking the transplant. The goal isn’t to keep levels at one fixed number. It’s to find the sweet spot for YOU-and adjust as you age, gain weight, or get sick.
Early after transplant, you might get blood draws twice a week. After a year, maybe once a month. But if you get sick, start a new medication, or feel off, your doctor will check levels again. Never stop or change your dose without talking to your transplant team.
When and How to Taper Off
Most patients stay on at least two immunosuppressants for life. But some can reduce their dose over time. This is called minimization or withdrawal.Doctors might lower steroid doses after 3 to 6 months. Some patients can even stop calcineurin inhibitors if they’re low-risk and stable. But this isn’t for everyone. It only happens under close supervision, with frequent biopsies and blood tests to catch rejection early.
There’s no such thing as being ‘cured’ of needing immunosuppressants. Even if you’ve had your transplant for 10 years and feel great, your immune system hasn’t forgotten. Stopping meds suddenly can trigger rapid rejection. Symptoms? For a kidney: less urine, swelling. For a liver: yellow skin, belly pain. For a heart: shortness of breath, fatigue. These aren’t side effects-they’re warning signs.
What Happens If the Transplant Fails?
If your organ fails, you’ll need to go back on dialysis or get another transplant. At that point, continuing immunosuppressants doesn’t make sense. The drugs won’t save the organ, and they’re still hurting your body.Doctors will slowly reduce your dose over weeks. Stopping cold turkey can cause a dangerous immune rebound, leading to inflammation or even organ damage. Always work with your team to taper safely.
What’s Next? Personalized Medicine and Hope
The future of transplant medicine isn’t just about stronger drugs. It’s about smarter ones.Some centers are now using blood tests to measure immune activity-not just drug levels. This lets them personalize dosing. A patient with low rejection risk might get 50% less tacrolimus without higher rejection rates. That means fewer side effects and better quality of life.
Researchers are also exploring tolerance induction-teaching the immune system to accept the transplant without drugs. Early trials show promise, but it’s still experimental. For now, the best tool we have is careful, consistent use of today’s medications.
Transplant survival has improved dramatically. But living well after transplant means more than just taking pills. It means showing up for appointments. Monitoring your health. Asking questions. Being honest about missed doses. It’s a daily commitment. But for most, it’s worth it. Because with these drugs, you get more than extra years. You get life.
Can I stop taking immunosuppressants if I feel fine?
No. Feeling fine doesn’t mean your immune system isn’t quietly attacking your transplant. Stopping these drugs-even for a few days-can lead to sudden rejection, which may cause permanent organ damage or death. Always consult your transplant team before making any changes.
Which immunosuppressant has the least kidney damage?
mTOR inhibitors like sirolimus and everolimus are generally less toxic to the kidneys than calcineurin inhibitors (cyclosporine and tacrolimus). However, they come with other risks like lung inflammation and poor wound healing. Your doctor will choose based on your overall health and organ type.
Why do I need antibiotics after a transplant?
Because your immune system is suppressed, you’re vulnerable to infections most people fight off easily. Antibiotics, antivirals, and antifungals are given for the first 3-6 months to prevent serious infections like CMV, pneumonia, or fungal infections that could damage your new organ.
How often should I get blood tests after a transplant?
In the first few months, you may need blood tests twice a week. After a year, monthly checks are typical. But if you get sick, start a new medication, or miss doses, your doctor will check sooner. Levels must be monitored to keep them in the safe range.
Can I drink alcohol while on immunosuppressants?
Moderate alcohol may be allowed, but it depends on your organ and medications. Alcohol can damage your liver, interfere with drug metabolism, and raise blood pressure. Many transplant centers recommend avoiding alcohol entirely, especially after liver or pancreas transplants.
Do immunosuppressants cause weight gain?
Yes, especially corticosteroids like prednisone. They increase appetite and cause fluid retention. Weight gain is common in the first year. Diet, exercise, and reducing steroid doses over time can help manage it. Never stop steroids on your own to lose weight-this can trigger rejection.
What should I do if I miss a dose?
If you miss a dose, take it as soon as you remember-unless it’s close to your next scheduled dose. Never double up. Call your transplant center for specific advice. Missing doses increases rejection risk, so use alarms, pill boxes, or apps to stay on track.
Are there natural alternatives to immunosuppressants?
No. There are no proven natural remedies or supplements that can safely replace immunosuppressants. Some herbs like St. John’s wort or grapefruit juice can interfere with drug levels and cause rejection or toxicity. Always tell your doctor about anything you’re taking, even vitamins.
How do I know if my transplant is being rejected?
Symptoms vary by organ. For kidneys: less urine, swelling, high blood pressure. For liver: yellow skin, dark urine, belly pain. For heart: fatigue, shortness of breath, irregular heartbeat. For lungs: cough, fever, trouble breathing. But rejection can happen without symptoms-that’s why regular blood tests and biopsies are critical.
Can I get vaccinated while on immunosuppressants?
Yes-but only certain vaccines. Avoid live vaccines like MMR, chickenpox, or nasal flu spray. Inactivated shots like flu, pneumonia, and COVID-19 are safe and strongly recommended. Talk to your transplant team before getting any vaccine to ensure it’s appropriate for your level of immunosuppression.

Janette Martens
i cant belive people still take these drugs... my cousin got a kidney and stopped after 2 years... she's fine. like, why do they keep you on this crap forever? #CanadaStrong
Marie-Pierre Gonzalez
Thank you for this comprehensive and vital overview. As a healthcare professional, I cannot stress enough the importance of medication adherence and regular monitoring. Please, always consult your transplant team before making any changes-your life depends on it. 🙏
Louis Paré
So let me get this straight-you're telling me we're chemically neutering people for life because we can't figure out how to make organs not get rejected? This isn't medicine. It's institutionalized chemical slavery. We're just patching a broken system with toxic bandaids.
Sydney Lee
I find it deeply concerning that so many patients treat immunosuppressants like aspirin. This isn't a lifestyle choice-it's a biological covenant. The fact that half of kidney recipients skip doses is a moral failure of medical education, not a pharmacological one. You wouldn't skip insulin. Why skip this?
oluwarotimi w alaka
they want you on these drugs forever so you keep coming back to the hospitals. big pharma owns the system. why do you think they dont want you off it? they dont want you to be healthy... they want you dependent. and dont get me started on the vaccines... theyre just testing new viruses on us.
Debra Cagwin
This is such an important post. To anyone reading this: you're not alone. The daily grind of pills, blood draws, and fear is real-but you're stronger than you know. Small wins matter. One pill taken. One appointment kept. One day of feeling okay. That’s victory. Keep going. 💪❤️
Celia McTighe
I had a liver transplant 8 years ago. The steroids made me gain 60 lbs and I cried every day for a year. But now? I hiked Mount Rainier last summer. I’m alive. I’m here. And yeah, I take my meds. Every. Single. Day. 🌲❤️
Ryan Touhill
It's fascinating how modern medicine has turned transplant recipients into bio-engineered subjects. We’ve moved from survival to optimization. But at what cost? The psychological toll of lifelong pharmacological dependency is rarely discussed. You’re not just managing rejection-you’re managing identity.
Teresa Marzo Lostalé
I’m 12 years post-kidney. I still get anxious every time I miss a dose. But I also still get to watch my daughter grow up. That’s worth every pill, every blood test, every scary night. Don’t let fear make you forget the gift. 🌅