There’s no such thing as a vaccine generic in the way we think of generic pills. You can’t just copy a vaccine the way you copy a cholesterol drug. Vaccines are living systems, not chemicals. They’re made from viruses, bacteria, or mRNA instructions - things that change with every batch, every factory, every temperature shift. That’s why a ‘generic’ flu shot isn’t like a generic ibuprofen. It’s not a copy. It’s a whole new product, built from scratch.
Why Vaccines Can’t Be Generic Like Pills
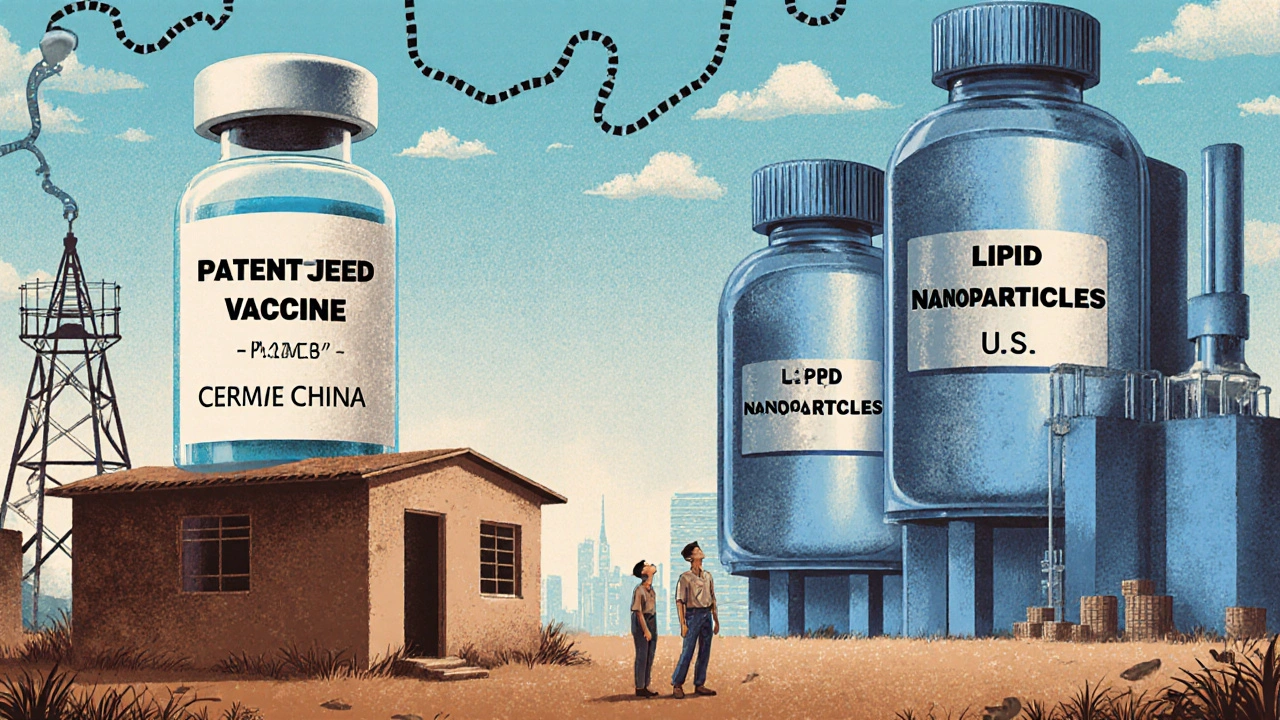
Generic drugs work because they’re simple molecules. If you know the chemical formula, you can make the same thing in a different lab. Vaccines? Not even close. They need live cells, precise fermentation tanks, sterile environments, and ultra-cold storage. One dose of an mRNA vaccine, like the ones used for COVID-19, requires dozens of specialized ingredients - including lipid nanoparticles that only five or seven companies worldwide can make. Even if you get the recipe, you can’t just buy the parts. Many are controlled, patented, or in short supply.The U.S. FDA doesn’t even have a shortcut process for vaccines like it does for pills. For a generic drug, you file an ANDA - a streamlined application. For a vaccine? You need a full Biological License Application. That means running new clinical trials, proving safety and effectiveness from the ground up. It takes years. It costs hundreds of millions. And it’s not just about the science - it’s about the factory.
The Factories That Don’t Exist
Building a vaccine plant isn’t like opening a pharmacy. It’s a $500 million project that takes five to seven years. You need biosafety level 2 or 3 labs, temperature-controlled rooms that can hit -70°C, and supply chains that don’t break when a single shipment of lipid nanoparticles gets stuck at customs. Only a handful of countries have the infrastructure. India has 11 major vaccine factories, including the Serum Institute, which makes more doses than any other place on Earth - 1.5 billion a year. But even that wasn’t enough in 2021.When the pandemic hit, high-income countries bought up 86% of the first billion doses. Africa, which produces 60% of the world’s vaccines by volume, imported 99% of its own. That’s not a mistake. It’s a system designed that way. Vaccine manufacturing is concentrated in just five companies: GSK, Merck, Sanofi, Pfizer, and Johnson & Johnson. Together, they control 70% of the global market. They don’t compete on price the way generic drug makers do. They set prices, and countries either pay or go without.
India: The Hidden Engine, But Not the Owner
India is the backbone of global vaccine supply. It makes 90% of the world’s measles vaccine. It supplies 60% of all vaccines used by the WHO. It produces the AstraZeneca shot for under $4 a dose - less than half what Western companies charge. But here’s the catch: India doesn’t own the technology. It licenses it. And when India had its own COVID wave in 2021, it stopped exporting. That cut global supply by half. No one had backup.Even worse, India imports 70% of its vaccine raw materials from China. That means when China tightens export rules, or the U.S. blocks shipments of critical lipids during a crisis, India’s production slows - and so does the world’s. Indian manufacturers are experts at scaling, but they’re not in control of the inputs. They’re assembly lines for someone else’s design.

Who’s Trying to Fix This?
The WHO set up a mRNA technology transfer hub in South Africa in 2021, with help from BioNTech. It was supposed to be the start of something new - local production, for Africa, by Africa. Three years later, it’s making mRNA vaccines. But only 100 million doses a year. That’s less than 1% of global need. The delay? Not because of lack of skill. It was because they couldn’t get the right machines. The right chemicals. The right training. One machine for mixing lipids cost $2 million. No supplier could deliver it on time.The African Union wants to get to 60% self-sufficiency by 2040. That requires $4 billion in investment. That’s not a small number. It’s more than the entire annual health budget of many African nations. And without political will, without long-term funding, without guaranteed buyers, no one will build the factories. Why invest $500 million if you don’t know if you’ll sell 10 million doses a year?
The Price of Inequality
In 2021, Médecins Sans Frontières found that 83% of the 1.1 million COVID vaccine doses sent to Africa went to just 10 countries. Twenty-three African nations had vaccinated less than 2% of their people. Meanwhile, in the U.S. and Europe, boosters were being offered to healthy teenagers. The same vaccine. The same science. Different access.Even when prices are lower, the system doesn’t work. Gavi, the global vaccine alliance, pays $10+ per dose for pneumococcal vaccines - even though the cost to produce them is under $2. Manufacturers say they need to recoup R&D. But R&D for these vaccines was often funded by public money. The Gates Foundation, the WHO, and governments paid for the science. Now, the same companies charge high prices to the poorest countries.

What’s the Real Barrier?
It’s not lack of knowledge. It’s not lack of will. It’s capital. It’s control. It’s a global system built for profit, not for people.There are no true vaccine generics because the system doesn’t allow them. Even if a country builds a factory, it still needs licenses, tech transfer, raw materials, and buyers. And the big players aren’t eager to share. They’ve spent decades protecting their patents, their supply chains, their pricing power. The pandemic showed us how fragile that system is. But it didn’t break it. It just exposed it.
India can make vaccines at scale. South Africa can learn to make mRNA. Brazil and Indonesia have the labs. But without guaranteed demand, without fair pricing, without open access to materials and tech - none of it scales. The world doesn’t need more patents. It needs more factories. More partnerships. More transparency.
For now, if you’re born in a low-income country, your chance of getting a vaccine isn’t based on need. It’s based on where your country sits in a global hierarchy of power, money, and supply chains. That’s not science. That’s politics.
What’s Next?
The U.S. FDA’s 2025 pilot program to fast-track generic drugs made in America shows a shift - but only for pills. No similar program exists for vaccines. Meanwhile, the WHO keeps pushing for tech transfer. Gavi keeps negotiating prices. But the gap keeps growing.By 2025, low- and middle-income countries will still be 70% dependent on imported vaccines, according to Gavi. That’s not progress. That’s the same problem, just slower.
The solution isn’t more meetings. It’s more factories. More funding. More rules that say: if public money paid for the science, the product must be accessible. Not just affordable. Accessible. In every country. On time. With the cold chain. With the trained staff. With the trust.
Until then, ‘vaccine generics’ will remain a myth. And millions will keep waiting.

Maria Romina Aguilar
I don't get why people think this is a new problem. Vaccines have always been this way. It's not about science-it's about who owns the patents. The system was built to keep profits high, not lives saved.
Denise Wiley
This is one of those posts that makes you want to hug someone and cry at the same time. 😭 We have the science. We have the people. We just don't have the will to share it. Why is that so hard to understand?
Hannah Magera
So if India makes so many vaccines, why can't they just make their own mRNA tech? Is it really just the machines? Or is it more about who owns the knowledge? I feel like there's a missing piece here.
Austin Simko
Bill Gates controls the supply chain. The WHO is his puppet. The whole thing is a scam to depopulate the third world.
Nicola Mari
I find it deeply offensive that anyone would suggest this is about 'inequality' rather than basic incompetence. If you can't build a factory, maybe you shouldn't be trying to make vaccines. It's not rocket science-it's biology. And biology requires discipline.
Sam txf
Let’s be real-this isn’t about access. It’s about entitlement. You think Africa deserves a vaccine like it’s owed a free meal? Wake up. The West built this system. We paid for the R&D. Now you want us to hand over the crown jewels for free? No thanks.
Michael Segbawu
India is just a factory for the west they make the shots but dont own the recipe and when they try to make their own the usa blocks the lipids like its some kind of war game and nobody talks about this because the media is owned by big pharma and we are all just sheep
Aarti Ray
We in India make billions of doses but we are not the ones who decide who gets what. When our own people were dying in 2021, we stopped exports. It was heartbreaking. But we had no choice. We are not villains. We are stuck in someone else's game.
Alexander Rolsen
You're romanticizing this. There's no moral high ground here. The world doesn't run on fairness. It runs on control. And the people who control the supply chains? They're not evil. They're just... smart. And you? You're mad because you don't have the same leverage.
Leah Doyle
This made me cry. I work in public health and I see the gaps every day. It's not just about money-it's about dignity. Everyone deserves to breathe easy during a pandemic. Not just the lucky ones. 🫂
Alexis Mendoza
I think the real question isn't 'why can't we make generics?' but 'why do we treat health like a commodity?' If we valued life the way we value profit, we'd have factories in every region. But we don't. We value control more.
Michelle N Allen
I mean I read all of this and I'm just like okay but like what am I supposed to do about it? I'm not a politician or a billionaire or even a scientist. I just want to not get sick. Maybe someone else should fix this?
Madison Malone
I really appreciate how you laid this out. It's not just about vaccines-it's about trust. When countries can't make their own, they lose control. And when they lose control, they lose hope. We need to build systems that honor that.
Graham Moyer-Stratton
The system works. The rich get protected. The poor get leftovers. That's how the world has always been. Stop pretending this is a moral failure. It's a natural outcome.
tom charlton
The structural inequities in global health infrastructure are not accidental. They are the result of decades of policy decisions prioritizing intellectual property rights over public health imperatives. To achieve equitable vaccine access, we must fundamentally restructure the global health governance architecture to include binding commitments to technology transfer, local manufacturing capacity, and price transparency.