Most people drink coffee without thinking twice. But if you’re on medication, that morning cup could be quietly undermining your treatment - or even putting you in danger. Caffeine isn’t just a pick-me-up. It’s a powerful chemical that interferes with how your body processes many common drugs. And the risks aren’t theoretical. People are ending up in emergency rooms because they didn’t know coffee could mess with their blood thinner, thyroid pill, or antidepressant.
How Caffeine Changes How Your Body Handles Medications
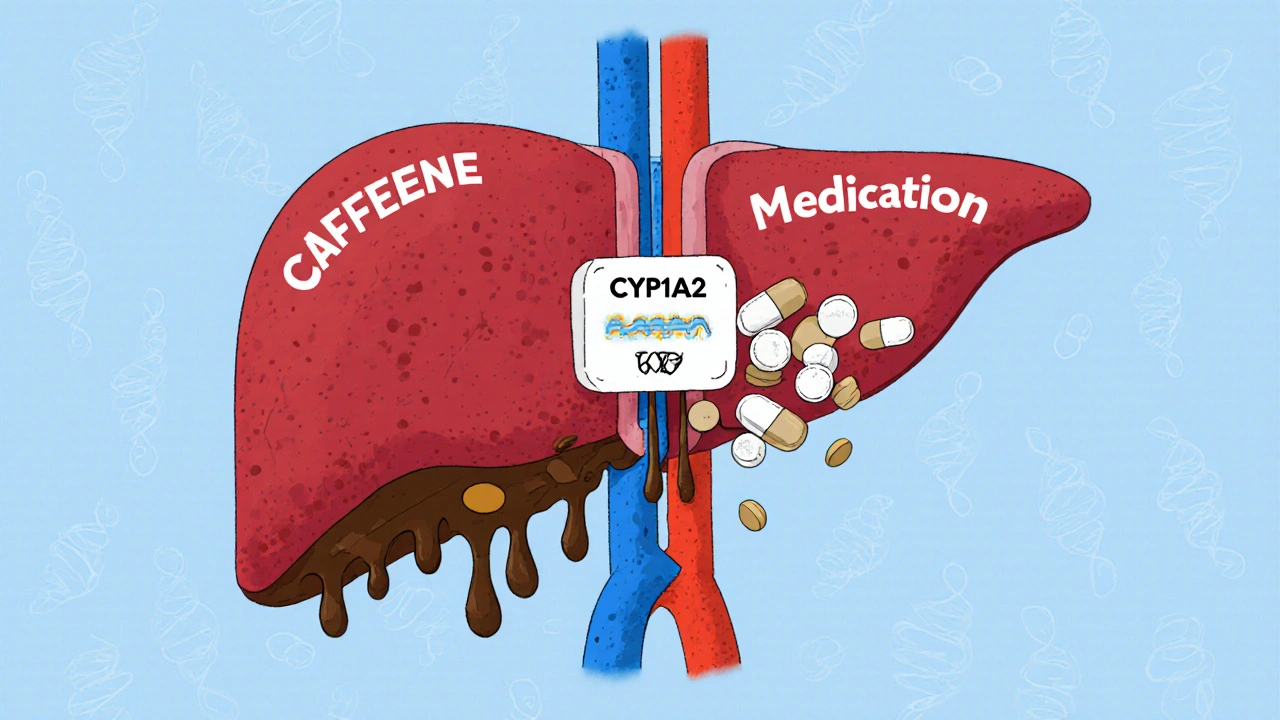
Caffeine doesn’t just wake you up. It’s metabolized by an enzyme in your liver called CYP1A2. That same enzyme breaks down more than 10% of all prescription and over-the-counter drugs. When caffeine is in your system, it competes for space on that enzyme. The result? Some drugs build up to dangerous levels. Others get cleared too fast, making them useless.
It’s not just about how much caffeine you drink - it’s about timing, genetics, and what else you’re taking. One study found that people with a certain genetic variation in CYP1A2 process caffeine up to four times slower. That means even one cup of coffee can linger in their system for over 12 hours, increasing the chance of interactions.
Warfarin and Caffeine: A Silent Bleeding Risk
If you’re on warfarin (Coumadin), caffeine isn’t just a concern - it’s a red flag. Research shows that drinking coffee while taking warfarin can raise your INR (a measure of blood clotting time) by 15 to 25% within 24 hours. That might not sound like much, but an INR above 4.0 puts you at serious risk of uncontrolled bleeding - from nosebleeds to internal hemorrhages.
A University of Michigan survey from early 2024 found that 41% of warfarin patients with unexplained high INR levels were consuming more than 200 mg of caffeine daily - roughly two large coffees. When they cut back, their INR stabilized. The FDA now requires warfarin labels to warn patients to keep caffeine intake consistent. Sudden increases - even just one extra cup - can trigger dangerous spikes.
Levothyroxine: Coffee Can Block Your Thyroid Med
Thyroid medication like levothyroxine needs to be absorbed in the upper intestine. Coffee, even black coffee without cream or sugar, can reduce that absorption by up to 55%. That’s not a small drop - it’s enough to turn a stable dose into an ineffective one.
One patient, who goes by ‘ThyroidWarrior2023’ on Reddit, took her levothyroxine with coffee for three weeks. Her TSH level - a key marker of thyroid function - jumped from 1.8 to 8.7. Her endocrinologist confirmed it was the coffee. She switched to taking her pill with water at least 60 minutes before her first cup. Within six weeks, her TSH dropped back to normal.
The American Thyroid Association now recommends waiting at least 60 minutes after taking levothyroxine before drinking coffee. Some experts suggest waiting 90 minutes for extra safety, especially if you’re still adjusting your dose.
Antidepressants: Caffeine Can Make Them Less Effective
SSRIs like fluoxetine (Prozac) and sertraline (Zoloft) are among the most commonly prescribed antidepressants. But caffeine can reduce their absorption by up to 33%, according to Harvard Health. That doesn’t mean you’ll feel worse right away - but over time, your symptoms might creep back.
Drugs.com has over 1,200 user reports linking caffeine with reduced antidepressant effectiveness. Sixty-three percent of those users reported increased anxiety, jitteriness, or sleep problems - signs that caffeine is overstimulating the nervous system while the drug struggles to work.
There’s an exception: fluvoxamine (Luvox). This SSRI actually slows down caffeine metabolism, causing it to build up in your body. That means if you’re on fluvoxamine, even one espresso could lead to heart palpitations, headaches, or nausea.
Heart Medications: Caffeine Can Cancel Out Your Blood Pressure Drug
Calcium-channel blockers like verapamil and diltiazem are used to treat high blood pressure and irregular heartbeats. But coffee can reduce their effectiveness by 25 to 30%. Dr. David Musnick from Harvard Health explains that caffeine competes with these drugs for absorption in the gut - so if you drink coffee too close to your pill, you’re not getting the full dose.
Patients on these meds are advised to take their medication at least two hours before or after coffee. Skipping that window can mean your blood pressure stays high - and your doctor might wrongly assume your medication isn’t working.
Even more dangerous is the combo of caffeine and adenosine or dipyridamole - drugs used in cardiac stress tests. If you’ve had coffee in the last 24 hours, the test can fail. That means you might need to reschedule, get a repeat test, or even miss a diagnosis. Cardiologists now routinely ask patients: “Did you have caffeine today?” before running these tests.
Theophylline: A Dangerous Mix for Asthma Patients
If you’re on theophylline for asthma or COPD, caffeine is a ticking time bomb. Both drugs are broken down by the same liver enzyme. When you add caffeine, theophylline levels can rise by 15 to 20%. That might sound like a good thing - until you start feeling your heart race, your stomach churn, or your hands shake.
In a 2024 study of 317 asthma patients on theophylline, 22% developed heart rates over 100 bpm after consuming more than 100 mg of caffeine (about one small coffee). One in five of those patients needed medical attention. Experts now recommend that theophylline users limit caffeine to less than 100 mg per day - and avoid energy drinks entirely.
Decongestants and Cold Meds: The Heart-Racing Duo
Pseudoephedrine, found in Sudafed and many cold remedies, is a stimulant. So is caffeine. When you combine them, your heart rate can jump 20 to 30 beats per minute. Dr. John Higgins from UT Southwestern calls this a “one-two punch.”
Patients with high blood pressure or heart conditions are especially at risk. One case study from the Mayo Clinic described a 58-year-old man who took Sudafed and had two cups of coffee. Within an hour, his systolic blood pressure spiked to 210 mmHg. He ended up in the ER. The Mayo Clinic warns that combining caffeine with ephedrine (a similar stimulant) increases the risk of hypertensive crisis by 47%.

What About Energy Drinks?
Energy drinks aren’t just coffee with sugar. They often contain 80 to 300 mg of caffeine per serving - sometimes more than two cups of coffee. And they’re loaded with other stimulants like taurine, ginseng, and guarana, which can also interfere with drug metabolism.
The FDA reports that 68% of serious caffeine-medication interactions reported between 2020 and 2024 involved energy drinks. These products are often consumed by young adults on ADHD meds, antidepressants, or heart drugs - people who don’t realize they’re playing Russian roulette with their health.
What Should You Do?
Here’s what works, based on real-world clinical guidance:
- Check your meds. Look at the label. If it says “avoid caffeine” or “interacts with stimulants,” take it seriously.
- Time it right. Take thyroid meds, blood pressure pills, and antidepressants at least 60 minutes before coffee. Wait two hours after taking verapamil or similar drugs before drinking.
- Limit caffeine. If you’re on warfarin, theophylline, or fluvoxamine, stick to under 100 mg per day - about one small coffee.
- Avoid energy drinks. They’re unpredictable. Even one can trigger a reaction.
- Talk to your pharmacist. They’re trained to spot these interactions. Ask: “Does my medication interact with caffeine?” Don’t assume it’s safe just because it’s not on the label.
Why Most People Don’t Know This
A JAMA Internal Medicine study in April 2024 found that 62% of patients on medications had no idea caffeine could interfere with their drugs. Even though 89% of adults drink caffeine daily, most doctors don’t ask about it. Pharmacists only started mandatory caffeine screening in 2023.
It’s not that the science is new. It’s that the warning hasn’t reached patients. Your doctor might not mention it because they assume you already know. But if you’re on any medication - especially for heart, thyroid, mental health, or blood clotting - you need to know.
What’s Changing Now
Things are starting to shift. The European Medicines Agency added specific caffeine warnings for new anticoagulants like edoxaban in March 2025. Epic Systems, one of the largest electronic health record providers, rolled out a caffeine-interaction alert in 47 hospitals in April 2025. Early results show a 29% drop in related adverse events.
By 2028, experts predict personalized caffeine guidance - based on genetic testing for CYP1A2 activity - will become standard. But you don’t have to wait. Right now, you can take control: know your meds, know your coffee, and talk to your pharmacist before you take your next sip.


Willie Doherty
The pharmacokinetic interference between caffeine and CYP1A2 substrates is well-documented in clinical literature, yet remains grossly under-communicated to the general population. The data presented here is methodologically sound, particularly the INR fluctuations in warfarin users and the 55% reduction in levothyroxine bioavailability. This is not anecdotal-it’s evidence-based pharmacology.
What’s concerning is the lack of standardized patient education protocols. The FDA’s labeling requirements are reactive, not proactive. We need mandatory pharmacist-led counseling at point-of-dispense, especially for high-risk medications like anticoagulants and thyroid hormones.
Darragh McNulty
THIS. IS. A. GAME. CHANGER. 🚨☕️ I had no idea my morning coffee was sabotaging my thyroid med! Switched to water + 1-hour wait… and my energy’s actually stable now. No more 3pm crashes. Thank you for sharing this 💪❤️
David Cusack
One might argue-though I hesitate to dignify it as such-that the entire premise rests upon a reductive interpretation of enzyme kinetics… but then again, the data from the University of Michigan survey… well, it does seem… statistically significant. One wonders, however, whether the sample size was adequately controlled for dietary flavonoids, which also inhibit CYP1A2…
And yet, the energy drink correlation-ah, that is the true menace. Not coffee. Not tea. Not even yerba mate. No, it’s the neon liquid sugar bombs marketed to adolescents with ADHD… and the FDA’s failure to regulate them as pharmaceutical adjuncts… is… frankly… unforgivable.
Elaina Cronin
As a clinical pharmacist with over 18 years of experience, I find this article both overdue and dangerously incomplete. You mention fluvoxamine’s inhibition of caffeine metabolism-but omit the critical point that this interaction can induce serotonin syndrome when combined with other serotonergic agents. That’s not a side effect-it’s a lethal cocktail.
Furthermore, you fail to address the systemic negligence of primary care providers who do not screen for caffeine intake during medication reconciliation. This is not patient ignorance-it’s institutional failure. Patients are not mind readers. We must do better.
Swati Jain
Let’s get real-this isn’t about coffee. It’s about pharmaceutical capitalism. Big Pharma doesn’t want you to know that a $2 cup of joe can interfere with a $150/month pill. They profit from re-prescribing, ER visits, and ‘non-compliance’ labels. The real villain? The $4 energy drink that’s 3x the caffeine of a Starbucks grande-and no warning label in sight.
Stop blaming the patient. Start regulating the product. And for god’s sake, put caffeine interaction alerts on every prescription bottle. This isn’t science-it’s corporate negligence dressed up as public health.
jim cerqua
Okay, so let me get this straight-my morning espresso is quietly turning my blood into soup, my thyroid meds are useless, and my antidepressant is basically a placebo because I drank coffee?!
And now you’re telling me I can’t even have an energy drink before my cardiac stress test?!
WHAT IS THIS, A NIGHTMARE?!
I’m not even gonna touch my coffee for a week. I’m going to drink water and stare at the wall and question every life choice that led me here.
Also, who the hell decided caffeine was a ‘safe’ substance? When did we stop being afraid of stimulants?!
Donald Frantz
Interesting breakdown. But I’m curious-how many of these interactions are dose-dependent? For example, does a single 50mg tablet of levothyroxine absorbed at 45% efficiency still maintain therapeutic levels? And are the cited studies controlled for time of day, food intake, and gastric pH?
Also, the 100mg caffeine limit for theophylline users-where’s the peer-reviewed validation? That number seems arbitrary. I’d like to see the confidence intervals from the 2024 study before accepting it as a universal guideline.
Sammy Williams
bro i literally took my zoloft with coffee every day for 2 years and never thought twice… just switched to drinking it 90 mins after my pill and i swear my anxiety’s been way less since. no joke. thanks for the heads up 😅
Julia Strothers
THIS IS A GOVERNMENT COVER-UP. The WHO, the FDA, the AMA-they all know caffeine is a weaponized stimulant designed to keep you dependent on pharmaceuticals. Look at the timing: right after the 2020 pandemic, they started pushing coffee as ‘healthy’ while quietly increasing antidepressant prescriptions.
And now they’re using ‘genetic testing’ as a distraction-because if you test your CYP1A2, you’ll have to pay for a $300 lab fee. Meanwhile, your coffee is still killing you.
They don’t want you to know that tea is safe. They don’t want you to know that decaf exists. They want you addicted to caffeine and pills. Wake up.
Erika Sta. Maria
Wait-so you’re telling me caffeine interferes with meds… but what about matcha? It’s got L-theanine so it’s ‘calm caffeine’ right? And what about yerba mate? It’s ancestral! And what about the fact that Ayurveda says coffee is tamasic so it’s already bad for your doshas? You’re ignoring the holistic framework!
Also, did you know that in 1987, a Tibetan monk drank coffee while on warfarin and his INR went to 12? That’s in the lost texts of the Himalayan Pharmacopoeia. You didn’t cite it because it’s not peer-reviewed… but it’s TRUE.
Also your spelling is wrong. It’s ‘levothyroxine’ not ‘levothyroxine’. I know because I’m a philosopher who reads Latin manuscripts. And also, the FDA is owned by Monsanto. Just saying.