Sedative Combination Risk Checker
Sedative Risk Assessment
This tool helps you understand the potential risks of combining sedative medications. Note: This is for educational purposes only and does not replace medical advice.
Risk Assessment Results
It’s not uncommon for people to take more than one medication to manage pain, anxiety, or sleep issues. But when you mix sedatives-like opioids, benzodiazepines, alcohol, or sleep pills-you’re not just adding effects. You’re multiplying danger. The result? A dangerous slowdown of your central nervous system that can stop your breathing, send you into a coma, or kill you without warning.
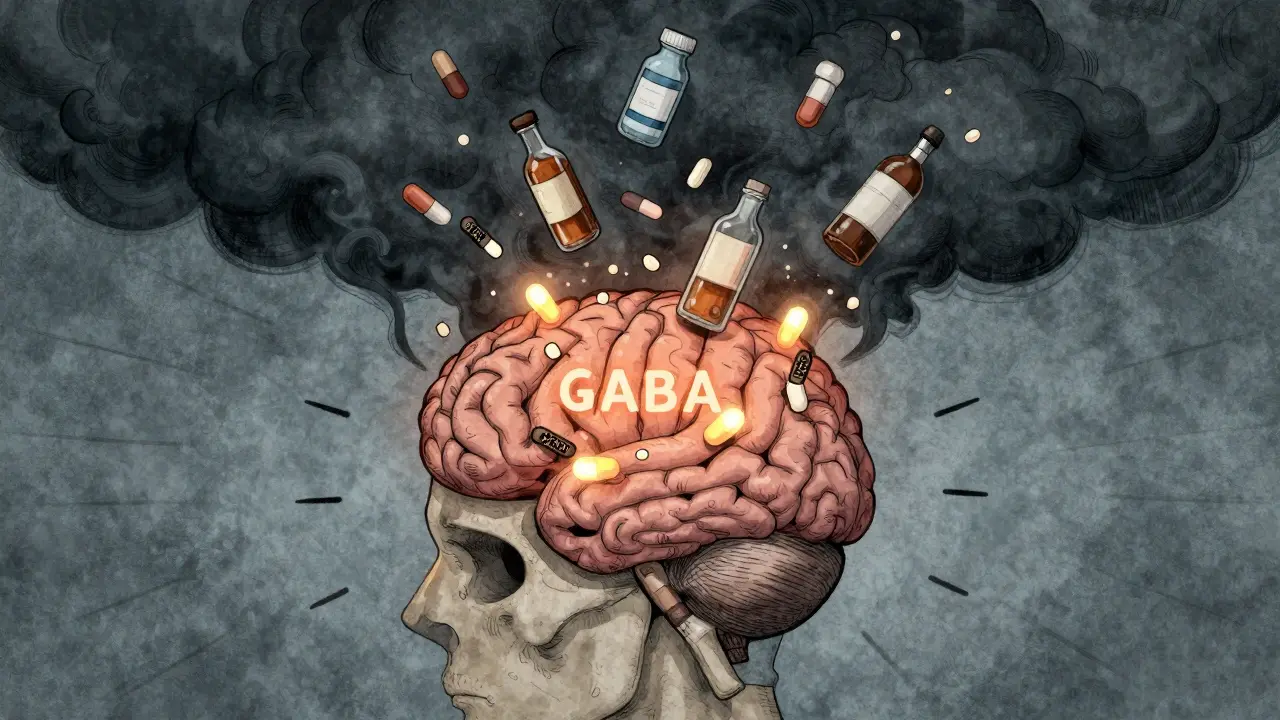
What Happens When Sedatives Combine?
Every sedative works by boosting GABA, a brain chemical that calms nerve activity. When you take one, it slows things down. Take two or three together, and that slowdown doesn’t just add up-it explodes. This is called CNS depression. Your brain stops sending clear signals to your lungs, heart, and muscles. Your breathing gets shallow. Your heart rate drops. Your blood pressure falls. Oxygen levels in your blood crash.
Studies show that when opioids and benzodiazepines are taken together, the risk of fatal overdose jumps by 2.5 to 4.5 times compared to using opioids alone. The FDA issued a warning in 2016 after reviewing hundreds of deaths tied to this mix. They required all opioid and benzodiazepine labels to carry a boxed warning-the strongest type-about the risk of respiratory failure and death.
Even over-the-counter sleep aids or alcohol can trigger this. One glass of wine with a prescription sleeping pill? That’s enough to slow breathing to 8-10 breaths per minute. Normal is 12-20. At 4-6 breaths per minute, your body starts shutting down. Oxygen saturation can drop below 85% in under 20 minutes. Brain damage can begin after just 4 minutes without enough oxygen.
Who’s Most at Risk?
It’s not just people who misuse drugs. Many are simply following their doctor’s orders. Elderly patients are especially vulnerable. Their bodies process drugs slower. Their brains are more sensitive. A 2023 study found that seniors on three or more CNS depressants had a 45% higher chance of being hospitalized after a fall. Hip fractures rose by 3.4 times. Many didn’t even realize they were at risk.
People with depression, chronic pain, or a history of substance use are also at higher risk. One study of 1,848 patients on long-term opioid therapy found that 39% of those with a past substance use disorder were also using benzodiazepines or alcohol. Even those without a history of addiction had a 29% rate of combining sedatives. Women were 1.7 times more likely to be prescribed multiple CNS drugs than men.
And it’s not just pills. Alcohol is the most common-and most dangerous-mixer. People don’t think of it as a sedative, but it’s one of the strongest. Taking a sleep pill and having a beer later that night? That’s a recipe for disaster. The effects don’t wear off on a schedule. They pile up.
The Long-Term Costs of Mixing
It’s not just about overdosing. Long-term use of multiple sedatives leads to a slow, silent decline. People report constant fatigue, weight gain of 12-18 pounds in a year, sexual dysfunction, and worsening depression. One in five users developed suicidal thoughts after six months of combined use. Sleep apnea jumped to 27% in long-term users. Cognitive decline accelerated-patients lost 5 points on memory and thinking tests over just one year.
These aren’t side effects you can ignore. They’re signs your nervous system is being worn down. Many patients don’t connect their foggy thinking, balance problems, or low mood to their meds. They assume it’s just aging. But it’s the drugs.

Common Dangerous Combinations
- Opioids + Benzodiazepines (e.g., oxycodone + alprazolam): Highest risk. Responsible for most fatal overdoses.
- Opioids + Alcohol: Slows breathing even more than opioids alone. Easy to do accidentally.
- Benzodiazepines + Sleep Medications (e.g., diazepam + zolpidem): Double sedation. Causes deep, unresponsive sleep.
- Barbiturates + Any CNS Depressant: Older drugs, still used in some cases. Extremely dangerous when mixed.
- SSRIs + Other Sedatives: SSRIs interfere with how other drugs are broken down. Can make sedatives stronger than expected.
Even seemingly harmless combinations-like a muscle relaxer with an anti-anxiety pill-can be risky. The danger isn’t always obvious until it’s too late.
What Doctors Are Doing About It
Health systems are waking up. The CDC advised doctors in 2016 to avoid prescribing opioids and benzodiazepines together. Since then, co-prescribing dropped by 15%. But it’s still happening. In 2020, over 10% of patients on long-term opioids still got benzodiazepines.
Tools are being built to stop it. Electronic health records now include clinical decision alerts that flag dangerous combinations. Hospitals using these systems saw a 28% drop in inappropriate sedative prescribing. The American Geriatrics Society lists 34 drugs that should be avoided in older adults because of fall and overdose risks.
Deprescribing-gradually reducing or stopping unnecessary meds-is now a standard practice. Patients who went through a structured deprescribing program saw a 32% drop in falls and a 27% improvement in memory over 12 months. Replacing long-acting benzodiazepines with non-benzodiazepine alternatives cut emergency visits by 19%.

What You Can Do
- Know what you’re taking. Write down every medication, including supplements and over-the-counter pills. Check labels for warnings like “may cause drowsiness” or “avoid alcohol.”
- Ask your doctor or pharmacist. Say: “Are any of my medications likely to interact dangerously?” Don’t assume they know all your meds-especially if you see multiple providers.
- Never mix with alcohol. Even one drink can turn a safe dose into a deadly one.
- Watch for warning signs. If you feel unusually drowsy, confused, dizzy, or have trouble breathing, stop taking the meds and call your doctor immediately.
- Don’t stop cold turkey. Some sedatives cause dangerous withdrawal. Always work with a professional to taper safely.
Many people don’t realize they’re at risk because they’re not “addicts.” They’re just trying to feel better. But safety isn’t about willpower-it’s about chemistry. Your body doesn’t care if you’re following prescriptions. It only reacts to the total amount of CNS depression.
The Future: Safer Prescribing
By 2025, most major electronic health record systems will automatically block dangerous sedative combinations unless a doctor overrides the alert with a detailed note. Some hospitals are testing genetic tests to see how fast a patient metabolizes drugs. People with certain gene variants break down sedatives slower-and are at higher risk. Testing could reduce dangerous interactions by 22%.
But until then, the responsibility falls on you. If you’re on more than one sedative, talk to your doctor. Ask if you really need all of them. Ask if there’s a safer way. Your life depends on it.
Can combining sedatives kill you even if you take them as prescribed?
Yes. Many deaths happen to people who take their medications exactly as directed. The danger comes from the interaction between drugs, not from taking too much of one. For example, taking a normal dose of oxycodone with a normal dose of alprazolam can slow breathing to dangerous levels-even if neither drug alone would cause harm at those doses.
How long does it take for sedative interactions to become dangerous?
It can happen within minutes to hours, especially if alcohol is involved. The effects build up over time, so you might feel fine after taking one pill, then feel extremely drowsy after a second or after having a drink. There’s no safe waiting period between sedatives. The risk is cumulative.
Are natural sleep aids like melatonin safe to combine with prescription sedatives?
Melatonin itself doesn’t depress the central nervous system like benzodiazepines or opioids, but it can still increase drowsiness. When combined with sedatives, it can make you feel more tired than expected and impair coordination. It’s not life-threatening like alcohol or benzodiazepines, but it adds to the risk. Always check with your doctor before mixing any supplement with prescription drugs.
What should I do if I think someone is overdosing on sedatives?
Call emergency services immediately. Signs include slow or irregular breathing, unresponsiveness, blue lips or fingertips, and extreme drowsiness. If naloxone is available and the person took an opioid, give it. But naloxone won’t reverse benzodiazepine or alcohol overdose. Only medical help can stop the breathing failure. Do not wait for symptoms to get worse.
Can I safely stop taking multiple sedatives on my own?
No. Stopping suddenly-especially benzodiazepines or barbiturates-can cause seizures, hallucinations, or life-threatening withdrawal. Always work with a doctor to create a gradual tapering plan. Many clinics now offer deprescribing programs designed to safely reduce or eliminate multiple CNS depressants over weeks or months.
Final Thought
Medications are meant to help. But when you stack sedatives, you’re not treating symptoms-you’re gambling with your breathing. There’s no such thing as a “safe mix.” The science is clear: combining these drugs increases risk exponentially. If you’re on more than one, don’t assume it’s fine. Ask. Check. Reconsider. Your life isn’t worth the risk.

RAJAT KD
One glass of wine with a sleep pill and you’re already in danger. This isn’t hype-it’s physiology. I’ve seen it in my clinic. People think they’re being careful. They’re not.
Alicia Hasö
Let me tell you about my aunt. She was 78. On oxycodone for arthritis, alprazolam for anxiety, and zolpidem for sleep. Her doctor said it was fine. She fell. Broke her hip. Spent six months in rehab. Then she died from pneumonia-her lungs had already been quiet for months. No one connected the dots. This isn’t rare. It’s routine. And we’re all pretending it’s not happening.
Doctors aren’t evil. They’re overwhelmed. But the system is broken. We need deprescribing as standard care, not a bonus feature. Every elderly patient should have a med review every six months-not just when they’re in crisis.
And stop calling it ‘compliance.’ This isn’t about following orders. It’s about survival. Your body doesn’t care if it’s ‘prescribed.’ It only knows chemistry. And chemistry doesn’t negotiate.
Elisha Muwanga
Of course this is dangerous. But let’s be honest-this is what happens when you let people medicate their way out of every problem. No discipline. No resilience. Just pop a pill, then another, then a glass of wine because ‘I had a rough day.’
We used to endure discomfort. Now we demand chemical anesthesia for life. This isn’t medicine. It’s surrender. And now we’re surprised when the system collapses under the weight of our own passivity?
Pooja Kumari
I just want to say-I get it. I’ve been on three of these at once. For years. I thought I was managing. I thought I was strong. But I wasn’t-I was just numb. I stopped feeling joy. Stopped laughing. Stopped wanting to leave the house. I thought it was depression. Turns out it was the cocktail.
My therapist asked me to write down every pill I took. I listed 11. Including melatonin and CBD oil. I thought they were ‘safe.’ They weren’t. They were the quiet accomplices.
I started deprescribing last year. Slowly. With a doctor who actually listened. It took six months to get off the benzos. I cried every day. But now? I sleep like a baby. Not because I took a pill-but because my body finally remembered how to rest.
If you’re reading this and you’re on more than one sedative? Please. Don’t wait until you’re in the hospital. Talk to someone. Even if you think you’re fine. You’re not. I was. And I almost didn’t make it.
You’re not weak for needing help. You’re brave for asking.
tali murah
Oh wow. Another ‘you’re all going to die’ PSA from the medical industrial complex. Let me guess-next they’ll tell us coffee causes anxiety and sunlight causes skin cancer.
People have been mixing alcohol and pills since the 1920s. And guess what? We didn’t all keel over. Some of us are still alive. Maybe the problem isn’t the drugs-it’s the fear-mongering?
Also, why is every single statistic tied to ‘studies’? Who funded them? Pharma? The FDA? Tell me the real numbers-not the ones that justify more regulation.
And why are women 1.7x more likely to be prescribed these? Maybe because they’re more honest about their pain? Or maybe because doctors still think women are ‘hysterical’ and need sedatives to ‘calm down’?
Stop treating patients like lab rats and start treating them like humans. Or better yet-stop prescribing so damn much in the first place.
Chris Kauwe
The real issue here is the erosion of biological sovereignty. The CNS is not a circuit board to be calibrated by pharmacological inputs. It is the seat of the soul’s interface with the material world-and when we flood it with GABAergic agents, we are not treating pathology-we are performing ontological sabotage.
The FDA’s ‘boxed warning’ is a bureaucratic performative act. It does not address the metaphysical collapse of agency that occurs when the individual outsources regulation of their neurochemistry to institutional authority.
Furthermore, the elevation of ‘deprescribing’ as a clinical virtue is a symptom of a culture that has lost its capacity for endurance. We no longer tolerate discomfort-we pharmacologize it.
And yet, paradoxically, we demand more drugs to fix the damage caused by the drugs we were told to take. This is not medicine. This is ritualized self-annihilation dressed in white coats.
Ian Long
I get why people are scared. I’ve been there. I took opioids after surgery, then got prescribed Xanax for anxiety. I didn’t think it was a big deal. Then I started blacking out. My wife found me slumped over the kitchen table at 3 a.m. I thought I was just tired.
My doctor didn’t connect the dots. Neither did I.
But here’s the thing-we’re not all going to die. Most of us just get foggy, tired, and confused. And we think it’s aging. It’s not. It’s the drugs.
What changed for me? I asked one question: ‘What if I took just one of these?’ I started with the sleep pill. Then the benzo. Then the opioid. Each time, I felt… clearer. Lighter. Like I’d been wearing a lead blanket.
It wasn’t easy. But it was worth it. You don’t need to be a hero. You just need to be curious. Ask your doctor. Ask your pharmacist. Ask your spouse. Don’t wait for a crisis. Ask now.
And if your doctor says ‘it’s fine’? Get a second opinion. Because sometimes, the system fails. And when it does, you’re the only one who can save yourself.
Phil Kemling
There’s a deeper layer here: we treat the body as a machine, and drugs as tools. But the CNS isn’t a gearbox. It’s a symphony. You don’t add more instruments to fix a wrong note-you listen. You adjust the tempo. You change the key.
Pharmaceutical intervention is often a band-aid on a broken rhythm. We suppress the symptom-drowsiness, anxiety, insomnia-without asking why the system is out of balance.
Is it trauma? Is it loneliness? Is it chronic stress? Is it the absence of meaning?
When we stack sedatives, we’re not just suppressing nerve signals-we’re silencing the body’s cry for help. And then we’re surprised when the silence becomes permanent.
Maybe the real danger isn’t the combination of drugs.
It’s the culture that tells us to numb ourselves instead of healing.
Lindsey Wellmann
😭 I just read this and started crying. My mom is on 4 of these. She says she’s fine. But she’s been falling more. She forgets my name sometimes. I think she’s scared to stop.
Thank you for writing this. I’m taking this to her doctor tomorrow. No more ‘it’s fine.’ Not anymore. 💔💊
Aron Veldhuizen
Let’s not forget: the entire pharmaceutical industry is built on the premise that every discomfort requires a chemical solution. This isn’t an accident. It’s business. Sedatives are profitable. Deprescribing? Not so much.
And yet, we treat patients like idiots who can’t manage their own nervous systems. We hand out prescriptions like candy and then act shocked when they overdose.
Also-melatonin isn’t ‘safe.’ It’s a hormone. Hormones don’t play nice with other hormones. And yes, it can amplify CNS depression when layered with benzodiazepines. The science is clear. But the FDA won’t regulate it because it’s ‘natural.’
So we have a system that bans alcohol in prescriptions but lets you buy 10mg of melatonin at Walmart like it’s candy. That’s not logic. That’s hypocrisy.
And don’t get me started on how SSRIs inhibit CYP enzymes and turn normal doses into toxic ones. No one talks about that. Because it’s complicated. And complexity doesn’t sell ads.
Jerian Lewis
If you’re taking more than one sedative, you’re not just at risk-you’re already failing. You’ve surrendered your autonomy to a system that profits from your dependence. You’re not a patient. You’re a revenue stream.
Stop asking for permission. Start asking why you need these at all.
And if you’re too scared to stop? That’s the drug talking. Not you.