Opioid Risk Assessment Calculator
This tool helps you understand your risk level for opioid-related complications based on the Opioid Risk Tool (ORT). Your risk score determines how frequently urine drug screens should be performed during treatment.
Your Risk Assessment Results
Recommended Testing Frequency
What your score means
A score of 0-2 points indicates Low Risk - you're at minimal risk for complications with opioid therapy.
A score of 3-4 points indicates Moderate Risk - you may need additional monitoring and support.
A score of 5 points indicates High Risk - you're at significant risk for complications and require intensive monitoring.
Important Note: This tool is based on the Opioid Risk Tool (ORT) used in clinical practice. It's designed for educational purposes and should not replace professional medical advice. Always discuss your individual situation with your healthcare provider.
When patients are prescribed opioids for chronic pain, doctors aren’t just trying to manage pain-they’re trying to keep them alive. Opioid misuse, diversion, and accidental overdose remain serious risks, even when medications are taken as directed. That’s why urine drug screens and risk stratification have become standard tools in opioid treatment. But these tests aren’t perfect. And using them wrong can hurt patients more than help them.
Why Urine Drug Screens Are Used in Opioid Treatment
Urine drug screens are not about punishment. They’re about safety. The goal is simple: confirm that a patient is taking the medication they were prescribed and not using other substances that could be deadly when mixed with opioids. The CDC reports that in 2021, over 80,000 of the 107,000 drug overdose deaths in the U.S. involved opioids. Many of those deaths happened because patients were mixing prescribed opioids with alcohol, benzodiazepines, or illicit drugs like fentanyl-sometimes without their doctor’s knowledge. Urine testing gives clinicians objective data. It answers questions like: Is the patient taking their oxycodone? Are they using cocaine or methamphetamine? Did they stop taking their buprenorphine? Without this information, doctors are guessing. And guessing in opioid therapy can be fatal.How Urine Drug Screens Work (And Where They Fail)
Most clinics start with a quick, cheap test called an immunoassay. These cost around $5 per screen and give results in hours. They’re good at spotting morphine, codeine, and some synthetic opioids. But they have major blind spots. For example, hydrocodone-a common prescription opioid-often doesn’t show up on standard opiate screens. Studies found that 72% of patients taking hydrocodone tested negative on immunoassays, even though they were taking their medication exactly as prescribed. That’s not patient noncompliance. That’s a flawed test. Fentanyl is another problem. Most routine urine screens can’t detect it because its chemical structure is too different from morphine. This means patients on fentanyl patches or lozenges can test negative, even if they’re taking the full dose. In one 2023 survey, doctors reported that nearly half their fentanyl patch patients were falsely flagged as non-adherent because of this. Confirmatory tests like gas chromatography-mass spectrometry (GC/MS) or liquid chromatography-mass spectrometry (LC-MS) fix these issues. They can identify exact drugs and metabolites, down to the nanogram. But they cost $25 to $100 per test and take days to process. Many clinics skip them because of cost or time, even when the initial screen looks suspicious.The Hidden Problem: False Negatives and Patient Trust
A negative test for a prescribed drug doesn’t mean the patient is lying. It often means the test is broken. A 2022 survey of over 1,200 pain specialists found that 68% saw false-negative hydrocodone results at least once a month. Patients who’ve been taking their medication correctly are told they’re “non-compliant.” Some lose their prescriptions. Others feel betrayed. One Reddit user, ChronicPainWarrior22, wrote: “I took my oxycodone every 6 hours like clockwork. My test came back negative. My doctor accused me of selling my meds. I cried for hours.” That’s not just unfair-it’s dangerous. When patients lose trust, they stop talking. They stop showing up. And that’s when overdoses happen. The same issue affects buprenorphine. Some immunoassays cross-react with other drugs, making it look like the patient is using something they’re not. In one study, 23% of patients on buprenorphine were wrongly punished because of false positives.
What’s New: Better Tests and Smarter Screening
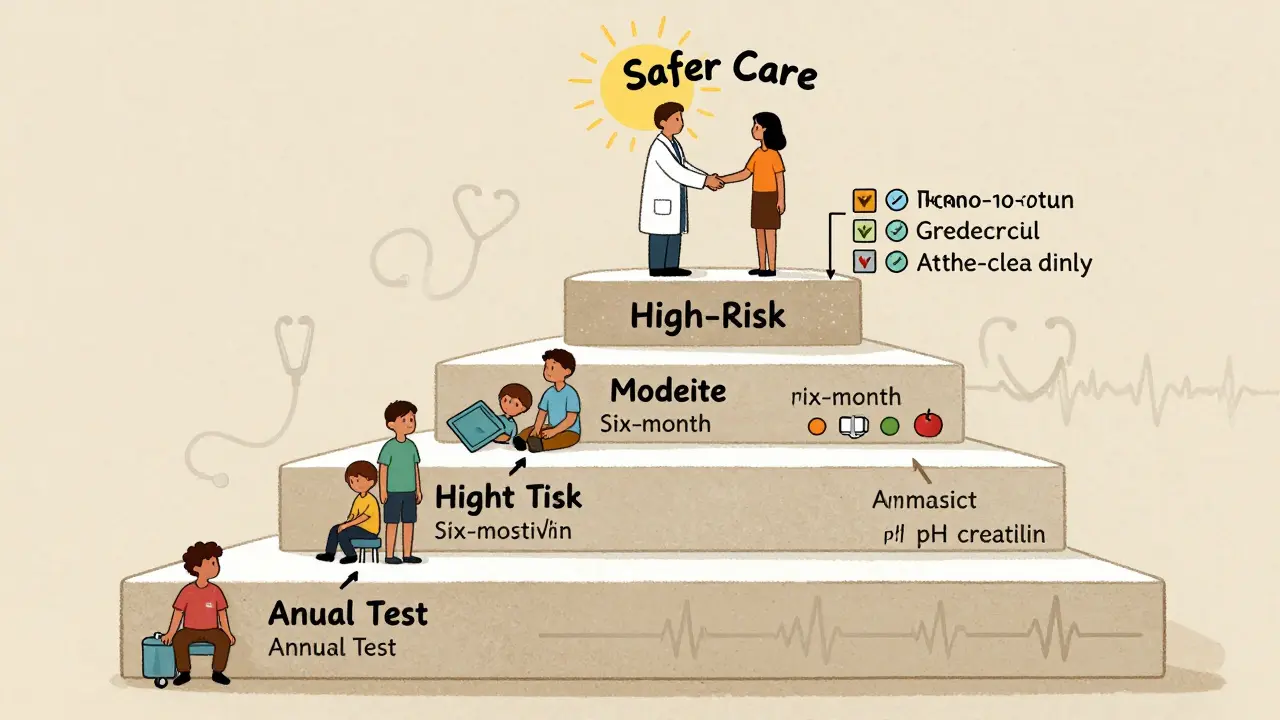
The tide is turning. In 2023, the FDA approved the first immunoassay specifically designed to detect fentanyl. It’s 98.7% accurate at detecting levels as low as 1 ng/mL. That’s a game-changer. Clinics that switch to this test can now confidently monitor patients on fentanyl patches without needing expensive confirmatory tests every time. Another big improvement is risk stratification. Instead of testing everyone the same way, doctors now use tools like the Opioid Risk Tool (ORT). It’s a five-question screening that asks about family history of substance use, personal history of mental health issues, age, and past drug misuse. Based on the score, patients are labeled low, moderate, or high risk. - Low-risk patients: Annual urine testWhat Clinicians Need to Know About Specimen Validity
A urine sample can be tampered with. Patients might dilute it with water, add chemicals to mask drugs, or even bring in someone else’s urine. That’s why every test should include a validity check. Standard checks look for:- Specific gravity (should be above 1.003-below that means diluted)
- pH (should be between 4.5 and 9.0-outside that range suggests adulteration)
- Creatinine (should be over 20 mg/dL-lower means substitution or dilution)
Who’s Paying for This? And How It’s Changing
The urine drug testing market hit $3.1 billion in 2022 and is growing fast. Medicare alone processed nearly 39 million tests in 2022. Reimbursement varies wildly: $20 for a basic immunoassay, up to $108 for full LC-MS panels. But money isn’t the only driver. Thirty-eight U.S. states now legally require urine testing for patients on high-dose opioids. Insurance companies are starting to tie coverage to testing compliance. That’s why 92% of pain clinics and 78% of primary care offices now use these tests regularly. Still, the big labs-Quest Diagnostics, LabCorp, BioReference, Aegis Sciences, and Millennium Health-control 87% of the market. Smaller clinics often have no choice but to use their panels, even if they’re outdated. That’s why awareness matters. Doctors need to know which drugs their lab can and can’t detect.What You Should Do If You’re on Opioids
If you’re prescribed opioids for chronic pain:- Ask your doctor which test they use. Is it a basic immunoassay or a confirmatory test?
- Ask if they check for fentanyl and hydrocodone specifically.
- Know your risk score. If you’ve never been assessed, ask for the Opioid Risk Tool.
- Keep a log of your doses and times. If your test comes back negative, you’ll have proof.
- Don’t assume a negative result means you’re in trouble. Ask for clarification.
The Bottom Line
Urine drug screens are not a magic solution. They’re a tool-one with serious flaws. Used blindly, they cause harm. Used wisely, they save lives. The best approach combines targeted testing based on risk, updated technology that detects modern opioids, and open communication between patient and provider. The goal isn’t to catch people doing something wrong. It’s to make sure they’re not dying because no one knew they were using something dangerous.Do urine drug tests prove if someone is addicted to opioids?
No. Urine tests only show what substances are present in the body at the time of testing. They can’t diagnose addiction. Addiction is a clinical diagnosis based on behavior, psychological symptoms, and impact on daily life-not on a single test result.
Why does my prescribed hydrocodone keep showing up as negative?
Many standard urine screens are designed to detect morphine and codeine, not hydrocodone. Hydrocodone is chemically different and often doesn’t trigger a positive result on basic immunoassays. You need a specific test for hydrocodone or a confirmatory test like GC/MS or LC-MS to detect it accurately.
Can I be penalized for a false positive on a urine test?
Yes, unfortunately. Some clinics still treat a false positive as noncompliance and may reduce or stop your prescription. That’s why it’s critical to ask for confirmatory testing if your result seems wrong. You have the right to request a more accurate test, especially if you’re taking your medication as prescribed.
Are blood tests better than urine tests for opioid monitoring?
No, not for routine monitoring. Blood tests show recent use-usually within hours. Urine tests detect use over the past 1-3 days, which is more useful for tracking adherence. Blood tests are only used in emergencies, like suspected overdose or when urine isn’t available.
How often should I be tested if I’m on long-term opioids?
It depends on your risk level. Low-risk patients (no history of substance use, stable mental health) typically need one test per year. Moderate-risk patients (past misuse or mental health conditions) should be tested every six months. High-risk patients (current or past addiction, high-dose opioids) need testing every three months, plus validity checks on each sample.
Is it legal for my doctor to stop my opioids because of a negative urine test?
Legally, yes-doctors can discontinue prescriptions based on their clinical judgment. Ethically, it’s questionable if they didn’t follow up with a confirmatory test or consider other explanations. If you believe your test was inaccurate, ask for documentation, request a retest, or seek a second opinion.


Shanahan Crowell
Man, I’ve been on oxycodone for six years, and I’ve had three false negatives on hydrocodone tests-each time, they nearly cut me off. I had to bring my pill bottle and a logbook to prove I wasn’t lying. It’s not about trust-it’s about flawed tech. Why are we still using 2005 screens in 2024?!
Kerry Howarth
Urine tests don’t diagnose addiction. They detect presence. That’s it.
Tiffany Channell
Let’s be real-these tests are just a way for clinics to control patients under the guise of safety. They don’t care about your pain. They care about liability. And if you’re poor, non-white, or on Medicaid? You’re already guilty until proven innocent.
Joy F
The entire opioid monitoring industrial complex is a grotesque performance of bureaucratic theater-where patients become data points, clinicians become compliance officers, and the very tools meant to save lives become instruments of systemic distrust. We’ve pathologized survival. We’ve turned medicine into a surveillance state wrapped in a white coat. And yet, we call this ‘evidence-based care’? The irony isn’t subtle-it’s screaming.
When your test comes back negative for hydrocodone, you’re not a liar-you’re a victim of pharmacological obsolescence. When fentanyl slips through because the lab’s machine was calibrated for morphine, it’s not your fault-it’s the system’s. We’ve outsourced clinical judgment to $5 dipsticks and then punish people for the machine’s ignorance.
And don’t get me started on risk stratification. The ORT? It’s a glorified personality quiz that conflates trauma with toxicity. A history of depression? High risk. A history of being poor? High risk. A history of being Black or Indigenous? De facto high risk. The algorithm doesn’t know the difference between vulnerability and villainy.
Meanwhile, the labs-Quest, LabCorp, Aegis-they’re not healthcare providers. They’re profit engines. They sell outdated panels because they’re cheaper to produce and easier to bill. The FDA approved a fentanyl-specific immunoassay? Great. But it’s not in 90% of clinics because the reimbursement doesn’t cover the cost. So we’re stuck in a loop: dangerous tech, underfunded care, and patients caught in the middle.
And yet, the narrative persists: ‘Just test more.’ No. Test smarter. Listen more. Trust more. The real crisis isn’t drug misuse-it’s the collapse of therapeutic relationship. When you tell a patient they’re noncompliant because their test missed a drug they’re literally holding in their hand, you’re not protecting them. You’re abandoning them.
It’s not about policing opioids. It’s about preserving dignity. And if we can’t do that, then we’ve already lost.
Haley Parizo
Let me tell you something about the American medical system-it doesn’t care if you’re in pain. It only cares if you’re profitable. You think they care about your fentanyl patch? No. They care about the $108 LC-MS bill they can charge. They care about the Medicare audit. They care about the paperwork. Your life? That’s just a footnote in their risk assessment spreadsheet.
And don’t even get me started on the ‘risk scores.’ You have anxiety? High risk. You lost a job? High risk. You’re a single mom? High risk. You’re a white guy with a college degree? Low risk. That’s not medicine. That’s prejudice with a stethoscope.
I’ve been on buprenorphine for eight years. I’ve never missed a dose. I’ve never sold a pill. But I’ve been accused of using cocaine because some immunoassay cross-reacted with my meds. I cried in the parking lot. My doctor didn’t apologize. He just ordered another test. And when it came back clean? He shrugged. ‘Well, we had to check.’
Check? Check what? That I’m human? That I’m not a criminal? That I deserve to breathe without being treated like a suspect?
They don’t need more tests. They need to look up from their screens and see us.
Ian Detrick
I work in a rural clinic. We do immunoassays because that’s all we can afford. We know they miss hydrocodone and fentanyl. We tell patients upfront. We don’t punish them for it. We just say, ‘We’ll flag this and get you a confirmatory test if needed.’ It’s not perfect, but it’s honest. And honesty builds trust. That’s what saves lives-not the test.
Angela Fisher
EVERYTHING is a government plot. Did you know the CDC is funded by Big Pharma? The whole opioid crisis was manufactured to push fentanyl patches and make people dependent on testing. The labs are owned by the same people who make the drugs. The ‘false negatives’? They’re designed to scare you into more tests, more meds, more money. I’ve seen it. My cousin’s doctor told him his test was ‘inconclusive’-then prescribed him a higher dose. Coincidence? I think not. They want you addicted so they can keep billing. They don’t want you better. They want you monitored.
And the ‘risk scores’? That’s just profiling. They label you high risk because you’re on Medicaid. They don’t care about your trauma. They care about your insurance code. I’ve been reading about this for years. It’s all connected. The testing, the prescriptions, the stigma-it’s all part of the same machine. And you? You’re just a number on a screen.
Don’t trust your doctor. Don’t trust the test. Don’t trust the system. They’re all lying to you.
Neela Sharma
In India, we don’t have urine tests for pain patients. We have trust. We have family. We have doctors who know their patients by name. Maybe the answer isn’t more technology-but less fear.
Shruti Badhwar
While the article presents a compelling case for improved diagnostic protocols, it remains critically insufficient in addressing the socioeconomic disparities that render these technologies inaccessible to marginalized populations. The assertion that ‘92% of pain clinics’ utilize testing neglects the fact that rural, uninsured, and underfunded clinics operate under entirely different constraints. The discourse on technological advancement must be coupled with structural equity initiatives, or else we risk exacerbating healthcare inequities under the guise of clinical rigor.
Brittany Wallace
I just want to say thank you for writing this. I’ve been silent for years because I was scared they’d take my meds. But reading this made me feel seen. I take my pills. I log them. I cry sometimes when the test comes back wrong. I’m not a bad person. I’m just trying to survive. And I’m so tired of being treated like a criminal.
Michael Burgess
Biggest thing I learned? Always ask what test they’re using. My doc used the basic one-missed my hydrocodone. I asked for LC-MS. He said ‘nope, too expensive.’ I went to a different clinic. Paid $40 out of pocket. Got my results in 2 days. Turned out I was clean. They apologized. Gave me a new script. Moral? Don’t let them skip the good test just because it costs more. You’re worth it.
Also-keep your pill bottles. Take pics of your schedule. If they doubt you, show them. You’re not asking for permission to be sick. You’re asking to be treated like a human.
And hey-if you’re on fentanyl? Ask if they can test for it. If they say no? Find a new doc. No excuse in 2024.
Liam Tanner
Just wanted to add that risk stratification works best when it’s not just a score-it’s a conversation. I use the ORT with my patients, but I always follow up with: ‘What does this mean to you?’ Sometimes the answer tells me more than the test ever could.
Palesa Makuru
Oh honey, you’re all missing the point. The real issue isn’t the test-it’s the fact that you’re even on opioids in the first place. Why didn’t you try yoga? Acupuncture? CBD? Or maybe just… stop being so dramatic about your pain? I mean, I’ve had back issues too, and I just gritted through it. You’re not special. You’re not broken. You’re just… weak. And now you’re addicted to pills because you didn’t have the willpower to suffer like a real adult.