Psoriasis & Insulin Resistance Risk Calculator
Enter your details and click Calculate to see your risk assessment.
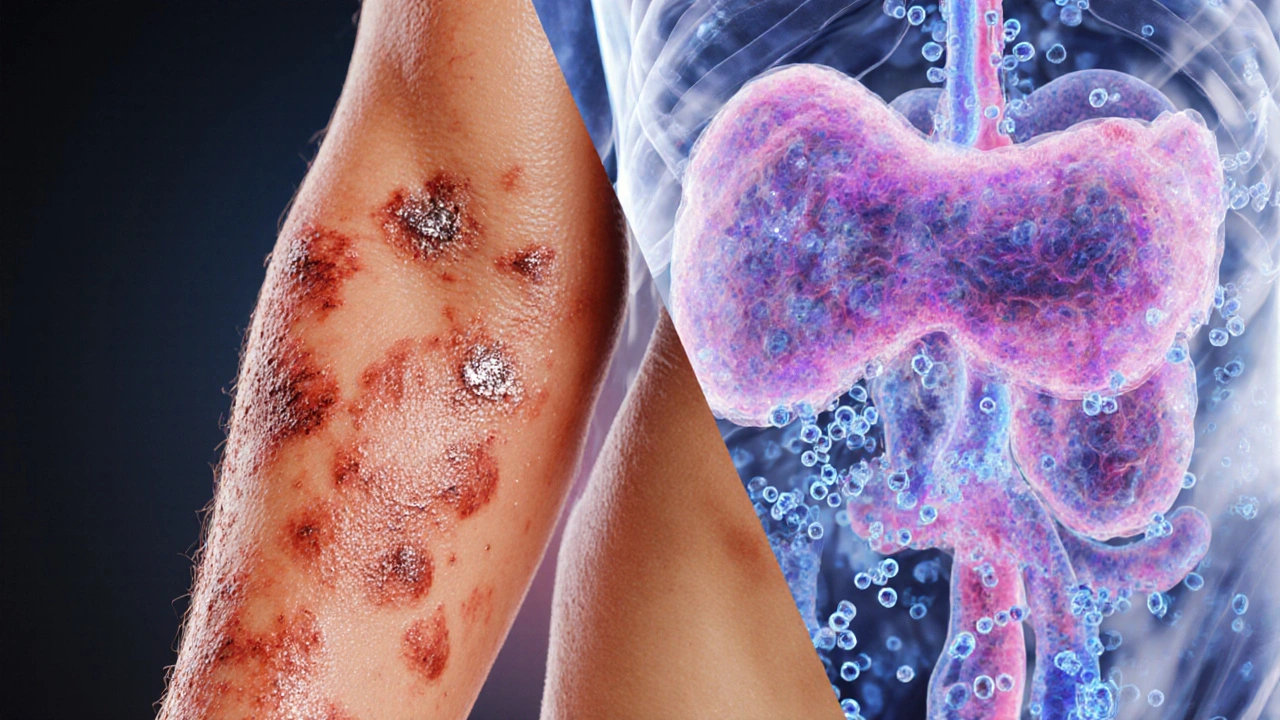
When it comes to chronic skin conditions, psoriasis is an immune‑mediated disease that causes red, scaly plaques on the skin. It affects about 2-3% of the global population, often appearing in early adulthood but sometimes later in life. At the same time, insulin resistance is a metabolic condition where the body’s cells respond poorly to insulin, forcing the pancreas to produce more of the hormone to keep blood sugar stable. While one lives on the surface and the other works deep inside the body, research over the past decade shows they frequently show up together.
Understanding the link between psoriasis and insulin resistance can change how you manage both conditions, from choosing the right medication to tweaking daily habits.
Key Takeaways
- Psoriasis and insulin resistance share common inflammatory pathways.
- People with moderate‑to‑severe psoriasis have a 30‑40% higher risk of developing type 2 diabetes.
- Weight loss, balanced diet, and regular exercise improve skin symptoms and insulin sensitivity.
- Some systemic psoriasis treatments (e.g., biologics targeting IL‑17) may also lower diabetes risk.
- Early screening for blood‑sugar abnormalities is advisable for anyone with chronic psoriasis.
What Is Psoriasis?
Psoriasis is more than a cosmetic issue; it is a chronic autoimmune disorder. The immune system mistakenly attacks healthy skin cells, accelerating their growth and causing the characteristic plaques. The most common form, plaque psoriasis, accounts for about 80% of cases. Symptoms can range from mild itching to severe pain and joint involvement, the latter known as psoriatic arthritis.
Genetics play a role - about 30% of patients have a first‑degree relative with the disease. Environmental triggers such as stress, infections, smoking, and certain medications can also flare the condition.
What Is Insulin Resistance?
Insulin resistance is the body’s reduced ability to respond to insulin, the hormone that moves glucose from the bloodstream into cells. When cells ignore insulin, the pancreas pumps out more of it, leading to higher circulating insulin levels (hyperinsulinemia). Over time, this strain can exhaust the beta cells, paving the way for type 2 diabetes.
Contributing factors include excess abdominal fat, sedentary lifestyle, poor diet, and genetics. It often shows up silently, detected only through fasting glucose or HbA1c tests.

How the Two Conditions Interact
Both psoriasis and insulin resistance are driven by chronic, low‑grade inflammation a sustained immune response that releases cytokines and other signaling molecules. Key cytokines such as tumor necrosis factor‑α (TNF‑α), interleukin‑6 (IL‑6), and interleukin‑17 (IL‑17) are elevated in psoriasis lesions and also interfere with insulin signaling pathways.
Research published in the Journal of Dermatological Science (2023) found that patients with severe plaque psoriasis had 1.5‑times higher serum IL‑6 levels, a cytokine known to blunt insulin receptor activity. This creates a vicious cycle: inflammation worsens skin, and the same inflammatory messengers impair cellular glucose uptake.
Moreover, the concept of metabolic syndrome a cluster of conditions including elevated blood pressure, high blood sugar, excess abdominal fat, and abnormal cholesterol levels often links both diseases. A 2022 meta‑analysis showed that more than 40% of people with psoriasis meet the criteria for metabolic syndrome, compared with 20% of the general population.
Shared Risk Factors
- Obesity excess body fat, especially around the waist - releases free fatty acids that fuel inflammation and worsen insulin resistance.
- Smoking - nicotine stimulates oxidative stress, aggravating both skin lesions and glucose metabolism.
- Unhealthy diet - high intake of saturated fats and sugars spikes insulin levels and can trigger psoriasis flares.
- Genetic predisposition - certain HLA‑C alleles increase psoriasis risk while other variants affect insulin signaling.
- Physical inactivity - lack of exercise reduces muscle glucose uptake and can lead to skin‑related stress.
Signs That You Might Have Both Conditions
Beyond the obvious skin plaques, watch for these clues that insulin resistance may be lurking:
- Persistent fatigue despite adequate sleep - a hallmark of poor glucose utilization.
- Frequent urination or increased thirst - early signs of elevated blood sugar.
- Darkened skin patches around the neck or armpits (acanthosis nigricans) - a visual cue of insulin resistance.
- Weight gain centered around the abdomen, even when diet appears stable.
- Elevated blood pressure or abnormal cholesterol numbers on routine check‑ups.
If you notice several of these alongside a psoriasis flare, consider asking your doctor for a fasting glucose or HbA1c test.
Managing the Overlap
Effective management targets both skin inflammation and metabolic health.
Lifestyle Interventions
- Weight loss: Even a 5-10% reduction in body weight can improve PASI (Psoriasis Area Severity Index) scores and insulin sensitivity.
- Balanced diet: Emphasize whole grains, lean proteins, omega‑3‑rich fish, and plenty of vegetables. The Mediterranean diet has shown a 20% reduction in psoriasis severity in a 2021 clinical trial.
- Regular exercise: Aim for 150 minutes of moderate aerobic activity weekly. Exercise improves muscle glucose uptake and releases anti‑inflammatory myokines.
- Quit smoking and limit alcohol: Both reduce systemic inflammation and improve medication efficacy.
Medical Therapies
Systemic psoriasis treatments can also influence insulin resistance:
- Biologics targeting IL‑17 medications like secukinumab and ixekizumab that block the interleukin‑17 pathway have been linked to modest improvements in fasting glucose.
- TNF‑α inhibitors (e.g., adalimumab) may lower insulin resistance by dampening the TNF‑α‑driven inflammation.
- Traditional systemic drugs such as methotrexate can improve metabolic markers, but require careful liver monitoring.
- Metformin - primarily a diabetes drug - is sometimes prescribed off‑label for patients with severe insulin resistance and may have added anti‑psoriatic benefits.
Always discuss potential side effects and drug interactions with a dermatologist or endocrinologist.
Monitoring and Follow‑Up
Regular blood tests are key. Recommended schedule for someone with moderate‑to‑severe psoriasis:
- Baseline fasting glucose, HbA1c, lipid panel, and liver function.
- Repeat every 6 months if any values are abnormal.
- Annual cardiovascular risk assessment, especially if you have additional metabolic syndrome components.
When to See a Doctor
If any of the following occur, book an appointment promptly:
- Rapid expansion of skin plaques or new joint pain - could signal psoriatic arthritis. \n
- Persistent high blood sugar readings (fasting >126 mg/dL) or HbA1c >6.5%.
- Sudden unexplained weight gain around the waist.
- Signs of cardiovascular strain - chest pain, shortness of breath, or high blood pressure.
Early intervention can prevent long‑term complications such as type 2 diabetes, heart disease, and severe skin damage.
Bottom Line
The connection between psoriasis and insulin resistance is rooted in shared inflammation, genetics, and lifestyle factors. Tackling one often helps the other. By staying aware of metabolic risks, adopting healthier habits, and working with healthcare providers on appropriate meds, you can keep both your skin and your blood sugar in check.
Frequently Asked Questions
Can psoriasis cause type 2 diabetes?
Psoriasis itself doesn't directly cause diabetes, but the chronic inflammation it creates increases insulin resistance, which can lead to type 2 diabetes over time.
Do biologic treatments improve insulin sensitivity?
Several studies show that IL‑17 and TNF‑α inhibitors reduce inflammatory markers that interfere with insulin signaling, often resulting in modest improvements in fasting glucose and HbA1c.
Is weight loss really effective for severe psoriasis?
Yes. A 10% body‑weight loss has been linked to a 30% drop in PASI scores in multiple trials, showing that reducing fat tissue cuts down inflammatory cytokine production.
Should I get screened for diabetes if I have mild psoriasis?
Screening is advisable if you have additional risk factors-family history of diabetes, obesity, or a sedentary lifestyle. For mild psoriasis alone, a baseline test every few years is reasonable.
Can diet alone control both conditions?
Diet is a powerful tool but rarely sufficient on its own. Combining a balanced diet with medical treatment and regular exercise yields the best outcomes.

karthik rao
While the article presents a superficial overview, it neglects the nuanced interplay between cytokine signaling and adipocyte metabolism. One must recognize that the pathophysiological cascade extends beyond mere BMI correlations. Moreover, the author's omission of recent IL‑17 inhibitor trials constitutes a glaring oversight. 🙄📚
Breanne McNitt
Great summary! I especially liked how the piece highlighted lifestyle modifications alongside pharmacotherapy. It really encourages a holistic approach.
Ashika Amirta varsha Balasubramanian
The interconnection between skin health and metabolic function mirrors the ancient principle of bodily harmony. When inflammation flares on the surface, it often signals deeper systemic imbalance. Embracing both dermatological care and metabolic monitoring can restore that equilibrium.
Jacqueline von Zwehl
I concur with the earlier points; ensuring proper punctuation even in medical writing aids clarity.
Christopher Ellis
They claim psoriasis drives insulin resistance but it's really just a correlation not causation the data is mixed
kathy v
Patriotic readers, let us confront the harsh reality that our nation's healthcare system frequently overlooks the connection between skin disorders and metabolic disease.
The article's bland approach betrays a complacent mindset that threatens the well‑being of our citizens.
We must demand comprehensive screening for insulin resistance in every psoriasis patient, not merely those who fit a narrow risk profile.
Our doctors should be equipped with the latest biologic therapies that have demonstrated reductions in systemic inflammation.
Failure to adopt these measures fuels a cycle of preventable complications that burden both families and the economy.
It is inconceivable that policymakers ignore robust data linking chronic inflammation to cardiovascular risk.
By championing public awareness campaigns, we can empower individuals to seek early intervention.
Lifestyle changes, such as adopting a Mediterranean diet, are not optional luxuries but essential components of treatment.
Exercise regimens tailored to each patient can dramatically improve insulin sensitivity.
Moreover, regular monitoring of HbA1c and lipid panels should become standard practice.
Those who dismiss these recommendations are effectively endangering the future health of the nation.
We owe it to our community to integrate dermatology and endocrinology services under one roof.
Such interdisciplinary clinics have already proven successful in reducing disease burden in several European models.
The United States must lead by example, not lag behind.
Only then can we claim true progress in combating the dual menace of psoriasis and insulin resistance.
Jorge Hernandez
Nice point! Keep an eye on your diet and you’ll see improvements 😊
Raina Purnama
Remember, cultural dietary habits can influence both psoriasis severity and insulin sensitivity, so consider traditional foods.
April Yslava
Our health is under constant attack by hidden elites who hide the true link between skin inflammation and metabolic sabotage. They push cheap meds while the real cure lies in restoring natural balance, yet the mainstream narrative keeps us in the dark.
Daryl Foran
Honestly the calculator is oversimplified it ignores genetic markers and stress levels
Rebecca Bissett
I feel deeply moved by the insights, they resonate profoundly, and they evoke a yearning for comprehensive care!
Michael Dion
Meh not impressed
Trina Smith
The delicate dance between epidermal health and glucose regulation invites us to contemplate the unity of bodily systems. 🌿🌟 Reflecting on ancient medicinal wisdom, we see that balance, not isolation, fosters healing.
josh Furley
Well, the data is pretty straightforward: psoriasis ↔ insulin resistance, but the jargon can be overwhelming 🤔. In simple terms, inflammation drives metabolic chaos.
Jacob Smith
Yo fam! This stuff is lit! Stay active, eat clean, and watch that skin glow! Keep pushin' forward, you got this! 💪
Chris Atchot
Your enthusiasm is commendable; however, note the correct spelling of “motivation” and “encouragement”.
Shanmugapriya Viswanathan
Everyone knows that our great nation has the best solutions for psoriasis and diabetes – just follow the proven American protocols! 🇺🇸
Rhonda Ackley
Alas, the tragic tale of missed opportunities unfolds before our eyes.
We watch as patients endure relentless itching while their blood sugars climb inexorably.
The world seems oblivious, wrapped in a veil of indifference.
Yet hope glimmers, like a distant lighthouse guiding weary souls.
If only we could unite dermatology and endocrinology, miracles might happen.
The burden of ignorance is heavy, pressing upon every heartbeat.
Let us raise our voices, not in anger but in compassionate resolve.
Together we can rewrite the narrative, turning pain into empowerment.
Sönke Peters
Interesting points all around. It’s worth considering both medical and lifestyle interventions.
Paul Koumah
Sure, because ignoring the science always works great.