When your nose is constantly stuffed up, your face feels heavy, and your head won’t clear - even after weeks of cold medicine - it might not be a cold at all. For people with allergies, persistent sinus symptoms are often a sign of allergy-related sinusitis. This isn’t just a bad cold that won’t go away. It’s a chronic inflammation triggered by your immune system’s reaction to everyday allergens like pollen, dust mites, or mold. And if you keep treating it like a regular infection, you’ll keep going in circles.
Why Allergies Make Sinusitis Worse
Allergies and sinusitis don’t just happen together - they feed each other. When you’re exposed to something you’re allergic to, your nasal lining swells, mucus thickens, and the tiny hair-like structures (cilia) that normally sweep out gunk get stuck. That’s when bacteria or fungi can take hold, turning a simple allergic reaction into a full-blown sinus infection. Studies show that up to 70% of people with chronic sinusitis also have allergic rhinitis. In fact, for many, the allergy comes first. You sneeze, you itch, you blow your nose - and over time, that constant irritation leads to blocked sinuses. The result? Pressure, pain, post-nasal drip, and fatigue that won’t lift. Unlike regular bacterial sinusitis, where antibiotics often work quickly, allergy-driven sinusitis doesn’t respond well to antibiotics alone. In fact, research shows antibiotics only help about 35-45% of the time in these cases. That’s because the root problem isn’t bacteria - it’s inflammation caused by your immune system overreacting.First-Line Treatments That Actually Work
The key to breaking this cycle? Treat both the allergy and the sinus inflammation - at the same time. Nasal corticosteroids are the most effective starting point. These aren’t the same as the steroids athletes use. They’re local sprays that reduce swelling right where it’s happening. Options like fluticasone (Flonase), mometasone (Nasonex), and budesonide (Rhinocort) are used once or twice daily. Don’t expect instant relief. It takes 2 to 4 weeks of daily use before you feel the full effect. But once it kicks in, studies show up to 65% reduction in symptoms - far better than oral antihistamines like cetirizine, which only help about 42% of the time. Saline nasal irrigation is another must. Using a neti pot or squeeze bottle with distilled or boiled water (never tap water) flushes out allergens and mucus. Do it once or twice a day. It’s cheap, safe, and backed by the American Academy of Allergy, Asthma & Immunology. Skipping this step is like trying to clean a dirty floor with a vacuum that doesn’t reach the corners. Environmental control matters more than most people realize. If you’re allergic to dust mites, use allergen-proof pillowcases. If mold triggers you, fix leaks and use a dehumidifier. A 2022 study found that reducing allergen exposure cuts sinus flare-ups by 40-60%. That’s like getting a free, daily treatment without a prescription.When Medications Aren’t Enough
If you’ve been on nasal sprays and saline for 4 to 6 weeks with no improvement, it’s time to think bigger. Allergy immunotherapy - commonly called allergy shots - is one of the most powerful long-term tools. It doesn’t just mask symptoms. It retrains your immune system. Over 3 to 5 years, weekly injections gradually reduce your sensitivity to allergens. Success rates? 60-70% of patients see a major drop in sinus infections. Compare that to just 25-30% with medication alone. It’s a big commitment - but for someone who gets sinusitis four or more times a year, it’s life-changing. For those with nasal polyps - soft, noncancerous growths in the nose that block airflow - newer biologic drugs are changing the game. Dupilumab (Dupixent), omalizumab (Xolair), and mepolizumab (Nucala) target specific parts of the immune system that drive inflammation. In trials, dupilumab reduced polyp size by 73%. But they’re expensive - around $3,500 a month without insurance - and only approved for severe cases.
When You Need to See an ENT Specialist
Not every sinus problem needs a specialist. But some signs mean you’re past the point of self-management. You should be referred to an ear, nose, and throat (ENT) doctor if:- Your symptoms haven’t improved after 4 to 6 weeks of proper treatment
- You have nasal polyps - visible or confirmed by endoscopy
- You’re having four or more sinus infections a year
- You’re experiencing vision changes, severe headaches, or swelling around the eyes
- You suspect fungal sinusitis - common in people with long-term allergies and mold exposure
What Not to Do
There are common mistakes that make things worse. Don’t overuse antibiotics. Most sinus infections - even in allergy sufferers - are viral or inflammation-based. Taking antibiotics unnecessarily doesn’t help and increases the risk of resistant bacteria. The Infectious Diseases Society of America recommends avoiding them for infections under 10 days unless symptoms are severe or worsening. Don’t use tap water in neti pots. In rare but serious cases, untreated tap water has carried Naegleria fowleri - a brain-eating amoeba. The CDC has documented cases from improper irrigation. Always use distilled, sterile, or previously boiled water. Don’t ignore aspirin-exacerbated respiratory disease (AERD). About 10-15% of people with chronic sinusitis and polyps also have this condition. Taking aspirin or NSAIDs like ibuprofen can trigger severe breathing problems. If you notice this pattern, you need specialized testing and possibly a desensitization program.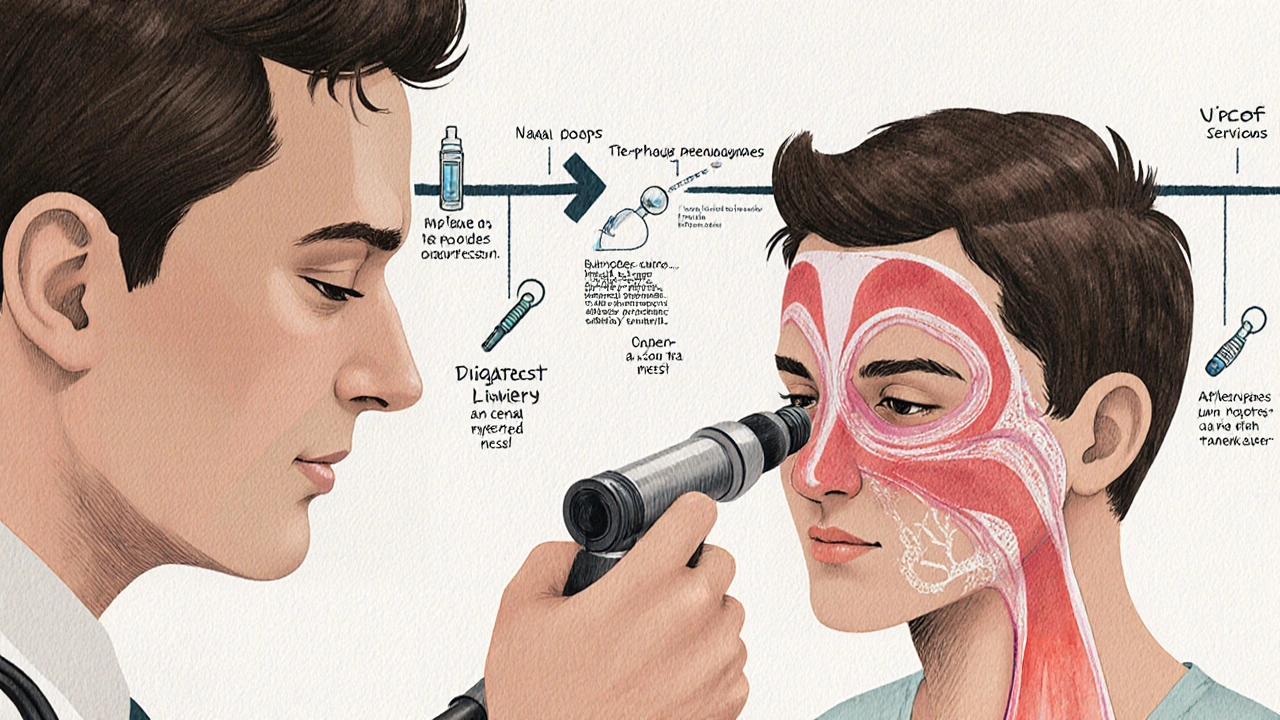
What’s New in 2025
The field is moving fast. In 2023, the FDA approved tezepelumab (Tezspire) for severe chronic sinusitis with nasal polyps. Early data shows a 56% drop in flare-ups. It’s another biologic option, especially for those who don’t respond to dupilumab. New research is also exploring intranasal antifungals for people in mold-heavy areas. A 2024 guideline now supports their use in selected allergy patients, with trials showing a 32% improvement in symptom scores. And scientists are looking at the sinus microbiome - the community of bacteria living in your nose. Early studies suggest that restoring healthy bacterial balance could cut antibiotic-resistant cases by nearly half in the next five years.The Big Picture
Allergy-related sinusitis isn’t just a nuisance. It’s a chronic condition that affects sleep, focus, mood, and quality of life. It’s responsible for over 12 million doctor visits a year in the U.S. alone, costing billions. The good news? You don’t have to live with it. The key is recognizing that this isn’t a one-size-fits-all problem. You need a plan that addresses both the allergy and the inflammation - and you need to stick with it. Nasal sprays take weeks. Immunotherapy takes years. But the payoff? Fewer infections, less pain, and more days where you can breathe without thinking about it. If you’ve been stuck in a loop of sinus infections, antibiotics, and temporary relief - it’s not your fault. It’s just the wrong approach. With the right tools and timing, you can break free.Is sinusitis always caused by allergies?
No. Sinusitis can be caused by viruses, bacteria, fungi, or structural issues like a deviated septum. But in people with allergies, it’s much more common and tends to be chronic. About 30-40% of all sinusitis cases are linked to allergic triggers, and in up to 75% of chronic cases, allergies preceded the sinus problems.
Can I treat allergic sinusitis with just antihistamines?
Antihistamines help with sneezing and itching, but they don’t reduce sinus swelling. For inflammation, nasal corticosteroids are far more effective. Studies show fluticasone reduces symptoms by 65%, while cetirizine only helps about 42%. Use antihistamines for allergy symptoms, but don’t rely on them for sinus pressure or congestion.
How long should I use nasal spray before expecting results?
Most nasal corticosteroids take 2 to 4 weeks of daily use to reach full effect. Many people stop too soon because they don’t feel better right away. But consistency is key - skipping days or using it only when symptoms are bad reduces effectiveness. Think of it like brushing your teeth: it works best when done regularly, not just when your mouth hurts.
Are biologic injections worth the cost?
For people with severe nasal polyps and chronic sinusitis who haven’t responded to other treatments, yes. Dupilumab can reduce polyp size by over 70% and cut the need for surgery or oral steroids. At $3,500 a month, it’s expensive - but many insurance plans cover it if you meet strict criteria. For those who qualify, the improvement in breathing, sleep, and daily function often outweighs the cost.
Can I prevent sinusitis if I have allergies?
You can significantly reduce your risk. Keep your home clean, use HEPA filters, avoid outdoor activities on high-pollen days, and shower after being outside. Saline rinses daily help flush allergens before they trigger inflammation. Allergy immunotherapy can cut future sinus infections by more than half over time. Prevention isn’t about perfection - it’s about consistent, smart habits.
When should I get an allergy test?
If you’ve had chronic sinusitis for more than 12 weeks, or if you have recurrent infections (4 or more per year), an allergy test is strongly recommended. Identifying your triggers lets you avoid them and helps your doctor choose the right treatment - like immunotherapy or targeted biologics. Testing is simple: skin prick or blood test. It’s not urgent, but it’s one of the most valuable steps for long-term control.


shubham seth
Okay so let me break this down like I’m explaining it to my cousin who still thinks Sudafed is a cure-all - allergies don’t just give you a runny nose, they turn your sinuses into a swampy, clogged drainpipe. And no, popping antibiotics like candy won’t fix it. You’re not fighting bacteria, you’re fighting your own immune system throwing a tantrum. Nasal sprays? Yeah, they’re slow as molasses, but if you stick with ‘em for a month? Game changer. I went from ‘I can’t sleep’ to ‘I forgot what a headache felt like.’
Kathryn Ware
OMG YES THIS!! 🙌 I used to be that person who’d take 3 antihistamines a day and still feel like my face was stuffed with cotton. Then I started using Flonase daily - even when I felt fine - and holy heck, it’s like my nose finally remembered how to breathe. Also, saline rinses? Non-negotiable. I use a neti pot every night before bed, and I swear by distilled water - I read about that brain-eating amoeba and now I’m terrified of tap water 😅
Gordon Mcdonough
Who the hell wrote this? This is just a drug company ad disguised as medical advice. Antibiotics work fine for me! I’ve been on them for years and I’m fine. Why are you pushing these expensive sprays and biologics? We don’t need all this fancy nonsense. Just take a decongestant and get over it. This is why America’s healthcare is broken - overmedicating people who just need to tough it out. 🇺🇸
Jessica Healey
soooo i tried the neti pot like 3 times and it felt like my brain was trying to escape through my eyeballs. i gave up. but then i started using those little squeeze bottles with the spout and it was like a whole different experience. also i swear by the allergen pillowcases - my husband didn’t believe me until he stopped waking up with a clogged nose. now he’s obsessed. also i cried when i saw the price of dupilumab. $3500?? no thank you, i’ll just keep sniffing.
Levi Hobbs
I appreciate the depth here. The point about nasal corticosteroids being underutilized because people expect instant results is spot-on. I stopped using mine after 10 days - thought it wasn’t working. Then I read a study that said 65% symptom reduction after 4 weeks. I restarted. Six weeks later, I was hiking without needing tissues. It’s not sexy. It’s not a miracle. But it’s science. Consistency beats hype.
henry mariono
Thanks for writing this. I’ve been dealing with this for years and felt like no one understood. I didn’t know about the connection between allergies and sinusitis until I read this. I’ve started the saline rinse and plan to talk to my doctor about immunotherapy. I’m not in a rush - but I finally feel like there’s a path forward. Just… thank you.
Sridhar Suvarna
Let me tell you something from India - we don’t have access to all these fancy sprays or biologics. But we do have tulsi leaves, steam with eucalyptus, and salt water rinses. The science is the same: reduce inflammation, flush allergens, calm the immune system. You don’t need a $3500 drug to breathe. Sometimes the oldest remedies are the most reliable. Just be consistent. That’s the real medicine.
Joseph Peel
As someone who moved from the Midwest to the Pacific Northwest, I went from seasonal allergies to year-round sinus hell. The shift in humidity, mold exposure, and pollen types was brutal. This article nailed it - environmental control isn’t optional. I installed a HEPA filter, sealed my windows, and now I use a humidifier only with distilled water. Small changes. Massive difference. No drama. Just facts.
Kelsey Robertson
Oh please. You’re just selling fear. ‘Chronic sinusitis’? Sounds like a buzzword invented by pharma to sell more drugs. I’ve had ‘sinus issues’ since I was 12. I’ve never seen a doctor. I blow my nose, drink tea, and go on with life. Why are you pathologizing normal human discomfort? People used to live without nasal sprays and biologics - and they didn’t die. Maybe the problem isn’t your sinuses… it’s your mindset.
Joseph Townsend
I WAS THE PERSON WHO CRIED IN THE PHARMACY WHEN I FOUND OUT DUPILUMAB WAS COVERED. I had polyps the size of grapes. Couldn’t smell coffee. Couldn’t sleep. Felt like I was suffocating in my own skin. Then I got the injection. Week 2? I woke up and realized I hadn’t woken up with a headache in 3 days. Week 6? I took a deep breath and it didn’t hurt. I didn’t know breathing could feel like a gift. This isn’t medicine. This is magic. And yes, it’s expensive - but so is losing your life to congestion.
Bill Machi
This is a textbook example of overmedicalization. Allergies? Just move to a dry climate. Sinusitis? Take a vacation. Why are we turning natural bodily responses into billion-dollar pharmaceutical industries? You want a solution? Stop living in moldy apartments. Stop eating processed food. Stop being lazy. Stop blaming everything on ‘inflammation.’ People used to live with stuffy noses. They didn’t need a $3000 shot to feel human.
Elia DOnald Maluleke
In the quiet hours before dawn, when the world is still and the air is heavy with the scent of rain on earth, I sit with my neti pot - not as a ritual of cure, but as a meditation of presence. The water flows not to erase the allergy, but to remind me that I am still here, still breathing, still fighting with grace. Science gives us tools, but it is the daily act of care - the choosing to rinse, to breathe, to persist - that becomes the true medicine. I am not broken. I am becoming.
satya pradeep
bro i tried the flonase for like 2 weeks and nothing happened so i stopped. then i read this and i started again. 3 weeks later i was like… wait i can breathe through my nose?? i didn’t even realize i’d been mouth breathing for years. also i didn’t know about the AERD thing. i take ibuprofen for headaches and now i’m scared. gonna get tested. thanks for the info. real talk.