Amiodarone Ocular Risk Calculator
This calculator estimates your risk of developing amiodarone-related eye side effects based on your age, daily dose, and medical history. Early detection can prevent vision loss.
Key Takeaways
- Amiodarone can cause a distinct set of eye problems, ranging from mild corneal deposits to sight‑threatening optic neuropathy.
- Most ocular side effects appear after 6‑12 months of therapy, but early signs may emerge sooner.
- Regular eye exams-baseline before starting the drug and at least annually thereafter-greatly improve the chance of catching reversible changes.
- If visual acuity drops or color vision fades, stop amiodarone promptly and involve an ophthalmologist.
- Risk is higher in patients over 60, those on high doses (>400 mg/day), or with pre‑existing thyroid or lung disease.
When doctors prescribe Amiodarone is a class III anti‑arrhythmic medication used to treat life‑threatening ventricular and supraventricular tachyarrhythmias, they focus on its powerful rhythm‑stabilizing effects. What often slips under the radar is its impact on the eyes. This review unpacks the mechanisms, incidence rates, and practical steps you can take to protect vision while staying on a drug that can save lives.
What Is Amiodarone and Why Is It Prescribed?
Amiodarone belongs to the Vaughan‑Williams class III group, meaning it prolongs the cardiac action potential by blocking potassium channels. It also inhibits sodium, calcium, and beta‑adrenergic receptors, giving it a broad anti‑arrhythmic profile. Because of its efficacy, it’s the go‑to agent for refractory ventricular tachycardia, ventricular fibrillation, and atrial fibrillation when other drugs fail.
Typical oral dosing starts with a loading phase of 800‑1200 mg/day for 1‑2 weeks, followed by a maintenance dose of 100‑400 mg/day. The drug’s half‑life can exceed 100 days, so steady‑state concentrations linger long after discontinuation.
How Amiodarone Affects the Eyes
Amiodarone’s eye toxicity stems from two main pathways:
- Lipid accumulation: The drug is highly lipophilic and deposits in corneal epithelium, leading to micro‑deposits visible on slit‑lamp exam.
- Oxidative stress: Reactive oxygen species damage retinal ganglion cells, contributing to optic neuropathy.
Both mechanisms are dose‑dependent, but even low‑dose patients can develop deposits because the drug accumulates in ocular tissues over months.
Common Ocular Side Effects
The spectrum of eye problems ranges from harmless to vision‑threatening. Below is a quick rundown:
- Corneal microdeposits (amiodarone keratopathy): Fine, brownish‑gold specks in the epithelial layer. Usually asymptomatic but may cause glare.
- Photophobia: Increased light sensitivity, often linked to corneal deposits.
- Blue‑gray skin discoloration: Not an eye issue per se, but it can affect the sclera and give a hazy appearance.
- Optic neuropathy: Progressive loss of visual acuity and color vision that may become irreversible if the drug isn’t stopped early.
- Retinal pigment epithelium changes: Rare, but can lead to visual field defects.
Incidence and Timeline
Incidence rates vary across studies because reporting methods differ. A 2023 multicenter cohort of 1,200 patients found:
| Side Effect | Incidence | Typical Onset | Reversibility |
|---|---|---|---|
| Corneal microdeposits | 70‑95 % | 3‑6 months | Usually reversible after discontinuation |
| Photophobia | 30‑50 % | Concurrent with deposits | Improves with dose reduction |
| Optic neuropathy | 0.5‑2 % | 12‑24 months | Often irreversible if not stopped early |
| Retinal changes | <0.5 % | 24‑36 months | Variable |
Notice the stark contrast: almost everyone gets corneal deposits, but optic neuropathy remains rare yet devastating.
Risk Factors That Heighten Eye Toxicity
Not every patient on amiodarone will develop eye problems. Certain characteristics increase the odds:
- Age > 60 years
- Maintenance dose > 400 mg/day
- Pre‑existing thyroid disease (hyper‑ or hypothyroidism)
- Concurrent pulmonary fibrosis or hepatic impairment, which alter drug clearance
- Long‑term therapy beyond 2 years
Screening these factors helps clinicians decide how aggressively to monitor.
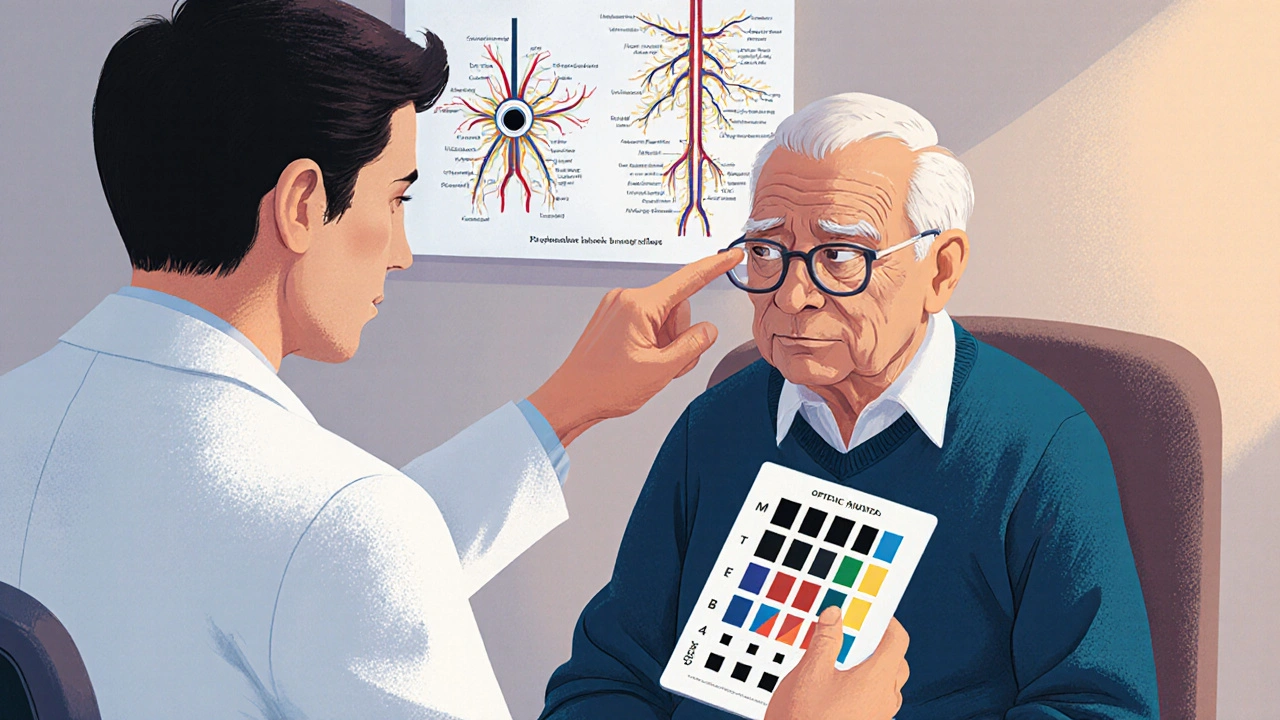
Monitoring Guidelines: What Eye Exams Should Look Like
Professional societies (e.g., American Heart Association, European Society of Cardiology) recommend a baseline ophthalmologic evaluation before starting amiodarone. Follow‑up exams should be scheduled as follows:
- Baseline slit‑lamp exam and visual acuity test.
- At 6 months, repeat the exam, paying attention to corneal deposits and color vision.
- Thereafter, at least annually, or sooner if the patient reports new visual symptoms.
A simple bedside test-checking red‑green color discrimination with Ishihara plates-can flag early optic nerve involvement.
Management Strategies: When to Reduce, Switch, or Stop
If corneal deposits appear but the patient is asymptomatic, the usual approach is to continue the drug while monitoring. Full‑dose reduction (e.g., from 400 mg to 200 mg daily) often diminishes glare.
However, any sign of optic neuropathy mandates immediate action:
- Discontinue amiodarone promptly.
- Switch to an alternative anti‑arrhythmic (e.g., sotalol or flecainide) if rhythm control remains necessary.
- Arrange urgent referral to a neuro‑ophthalmologist for visual field testing and possible corticosteroid therapy.
Evidence from a 2022 case‑series shows that stopping amiodarone within 4 weeks of symptom onset can stabilize vision in up to 70 % of patients.
Patient Education: What to Look for and Report
Empowering patients reduces delays. Encourage them to report any of the following:
- Blurry vision or difficulty reading signs.
- Loss of color discrimination, especially reds and greens.
- Unusual glare or halos around lights.
- Persistent eye discomfort that doesn’t improve with lubricating drops.
Reassure that corneal deposits are usually harmless, but emphasize that optic nerve issues are an emergency.
Special Populations
Pregnant women: Amiodarone crosses the placenta and can affect fetal thyroid. Ocular side effects are rarely reported in neonates, but the drug is generally avoided.
Elderly patients: Age‑related lens changes and dry eye disease can exacerbate glare from corneal deposits. Lower maintenance doses (<200 mg/day) are advisable when possible.
Summary of Best Practices
Putting it all together, the safest way to use amiodarone while protecting vision looks like this:
- Obtain a comprehensive eye exam before initiating therapy.
- Prescribe the lowest effective maintenance dose.
- Schedule follow‑up ophthalmology visits at 6 months and then yearly.
- Educate patients on early visual warning signs.
- Act quickly if optic neuropathy is suspected-stop the drug and switch class.
By following these steps, clinicians can harness amiodarone’s life‑saving rhythm control without compromising the patient’s sight.
How often should I have eye exams while on amiodarone?
A baseline exam before starting, a check at six months, and then at least once a year. If you notice any visual changes, see an eye doctor right away.
Can corneal deposits be removed?
The deposits usually fade after stopping amiodarone or lowering the dose. No surgical removal is needed; lubricating eye drops can improve comfort.
Is optic neuropathy reversible?
If caught early and the drug is discontinued promptly, some patients regain part of their vision. Late‑stage neuropathy often results in permanent loss.
Do lower doses eliminate eye risks?
Lower doses (<200 mg/day) reduce the likelihood of deposits and optic nerve damage, but they don’t erase the risk entirely. Regular monitoring remains essential.
What alternatives exist if I develop eye problems?
Depending on your arrhythmia, alternatives include sotalol, flecainide, or catheter ablation. Discuss with your cardiologist to find the safest option.


Abhinav Moudgil
Amiodarone truly exemplifies the double‑edged sword of modern pharmacotherapy-its capacity to stabilize life‑threatening arrhythmias is matched only by its proclivity for ocular intrigue. The review meticulously outlines how lipid‑laden corneal microdeposits manifest as a golden‑hued veil, often unnoticed until glare becomes a nuisance. More ominously, oxidative stress may herald optic neuropathy, a specter that demands vigilant surveillance. Instituting a baseline ophthalmic assessment before the first dose, followed by a six‑month reprise, aligns with best‑practice guidelines and can forestall irreversible loss. Ultimately, a balanced regimen-dose titration, patient education, and interdisciplinary collaboration-transforms risk into manageable nuance.
Kyle Garrity
Reading through the summary, I’m struck by how often clinicians might overlook the subtle visual complaints that patients report. The fact that corneal deposits affect up to ninety‑five percent yet seldom impair vision is a reminder that not every finding necessitates drastic action. However, the window for rescuing optic nerve function appears narrow; early color‑vision testing can make all the difference. I appreciate the emphasis on annual follow‑up, especially for those over sixty or on higher doses. It’s a solid, patient‑centered approach that bridges cardiology and ophthalmology.
brandon lee
Man the glare thing is real it messes up night drives but the deposits usually chill out on their own after you drop the dose.
Joshua Pisueña
Folks, let’s remember that Amiodarone’s ocular side‑effects are not a death sentence but a call to proactive care. By scheduling a slit‑lamp exam early, we catch microdeposits before they evolve into photophobia that disrupts daily life. Adjusting the maintenance dose can ease glare without compromising rhythm control, a win‑win for patients navigating both heart and sight health. Embrace the interdisciplinary dialogue-cardiologists, ophthalmologists, and patients together can demystify these visual phenomena.
Robert Urban
While the collaborative spirit is commendable, some might argue that the guidelines are overly cautious, potentially leading to unnecessary appointments and healthcare costs.
Stephen Wunker
The saga of amiodarone reminds us that medical triumphs often walk hand‑in‑hand with hidden shadows. In the quest to quell malignant arrhythmias, we harness a molecule that stubbornly lingers for months, infiltrating tissues beyond the heart. The ocular realm becomes an unsuspecting canvas where lipids settle like tiny constellations upon the corneal epithelium. One could liken these deposits to whispered signatures of a drug that refuses to vanish, a reminder of the body's intricate bookkeeping. Yet, the real philosophical quandary emerges when oxidative stress nudges retinal ganglion cells toward demise, threatening the very perception of color that defines our lived experience. Is it not paradoxical that a life‑saving therapy can imperceptibly erode one of our most cherished senses? This tension forces clinicians to adopt a dual‑lens perspective, balancing electrophysiological stability against visual fidelity. The literature, as the review aptly notes, underscores that optic neuropathy, while rare, carries irreversible consequences if ignored. Therefore, early detection through Ishihara plates is not merely a test but an ethical imperative. The patient’s narrative-blurred signage on a highway, fading reds in a sunset-should echo louder than any ECG strip. Moreover, the risk stratification matrix-age, dose, comorbid thyroid or pulmonary disease-offers a moral compass guiding frequency of surveillance. When the scales tip toward high‑risk, perhaps the physician should contemplate alternative anti‑arrhythmics, even if they lack amiodarone’s formidable efficacy. This substitution, however, is not a surrender but an act of stewardship, honoring the principle of “primum non nocere.” In practice, a collaborative care pathway involving cardiology, ophthalmology, and primary care can translate these philosophical musings into concrete protocols. Ultimately, the story of amiodarone ocular toxicity is a reminder that medicine is as much an art of listening to subtle visual cues as it is a science of electrical currents.
Jhoan Farrell
Thanks for the deep dive 🙏👀. It’s a humbling reminder that every prescription carries a ripple effect across the body. I’ll definitely share the color‑vision tip with my patients – those little red‑green plates can be lifesavers! 🌈✨
Jill Raney
Some claim the ocular findings are merely a placebo for the pharma industry.
bill bevilacqua
Well,, you see,, the evidence is quite clear,, that Amiodarone's ocular side effects are well-documented,, not some contrived myth,, and the ophthalmology community has published numerous studies!!
Grace Baxter
While many herald the routine eye exams as indispensable, I contend that the sweeping mandates often serve bureaucratic interests more than patient welfare. In an era where healthcare resources are stretched thin, mandating annual slit‑lamp evaluations for every amiodarone patient may divert attention from more pressing cardiac monitoring needs. Moreover, the data suggest that severe optic neuropathy remains a rarity, occurring in less than two percent of users, which raises questions about the cost‑benefit ratio of such pervasive surveillance. A more nuanced approach-targeting high‑risk cohorts based on age, dosage, and comorbidities-could preserve valuable clinical bandwidth while still protecting those most vulnerable. Ultimately, stewardship of medical resources demands that we resist blanket protocols and instead champion tailored, evidence‑driven strategies.