When you pick up a prescription at the pharmacy and see a different name on the bottle than what your doctor wrote, it’s natural to wonder: is this the same thing? The answer lies in a term you’ve probably never heard before - bioequivalent. It’s not about the label, the color, or the shape of the pill. It’s about what happens inside your body.
What bioequivalence actually means
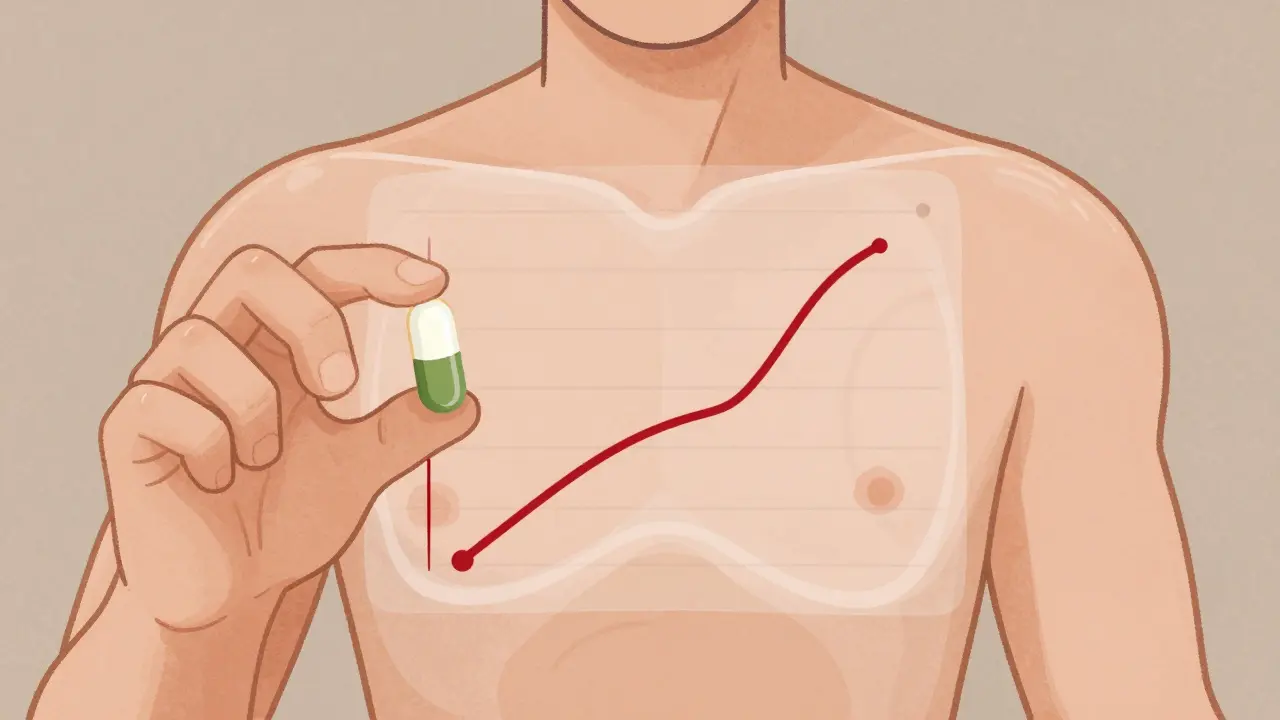
Bioequivalence doesn’t mean two drugs are chemically identical. It means they work the same way in your body. If you take a brand-name drug and a generic version, and both deliver the same amount of active ingredient into your bloodstream at the same speed, they’re bioequivalent. That’s it. No magic, no guesswork - just hard science.The U.S. Food and Drug Administration (FDA) defines it precisely: bioequivalence means there’s no significant difference in how fast and how much of the drug gets absorbed. The key measurements are Cmax (the highest concentration in your blood), tmax (how long it takes to get there), and AUC (how much drug your body is exposed to over time). For a generic to be approved, its results must fall within 80% to 125% of the brand-name drug’s numbers. That’s not a random range - it’s based on decades of data showing that differences smaller than 20% don’t change how well the drug works or how safe it is.
Why this matters for your health
You might think, “If it’s cheaper, is it weaker?” The answer is no - not for most drugs. About 90% of all prescriptions filled in the U.S. are for generic medications. That’s because bioequivalence standards let pharmacies swap brand names for generics without risking your treatment. The FDA has approved over 2,000 generic versions of drugs since 2020, and studies show they perform just as well in real-world use.But there are exceptions. For drugs where the difference between a helpful dose and a dangerous one is razor-thin - like warfarin, levothyroxine, or certain epilepsy medications - even small changes in absorption can matter. That’s why the FDA sometimes tightens the bioequivalence range to 90-111% for these drugs. And while most patients switch without issue, some do report changes. A 2021 study in JAMA Internal Medicine found a small number of epilepsy patients had breakthrough seizures after switching generics. That’s rare - but it’s why pharmacists often recommend sticking with the same generic manufacturer once you’ve found one that works.
Pharmaceutical equivalence vs. therapeutic equivalence
Don’t confuse bioequivalence with pharmaceutical equivalence. Two pills can have the same active ingredient, dose, and shape, but still differ in fillers, dyes, or coatings. That’s pharmaceutical equivalence. But if those differences change how the drug is absorbed, they’re not bioequivalent.Therapeutic equivalence is the gold standard. It means two drugs are both pharmaceutical equivalents and bioequivalent. The FDA labels these with an “AB” rating in the Orange Book - a public list of approved generic drugs. If your prescription says “AB,” you can swap it with confidence. If it says “BX,” the generic hasn’t been proven equivalent - and your pharmacist can’t substitute it without your doctor’s approval.

How bioequivalence is tested
Before a generic drug hits the shelf, the manufacturer must run a study in 24 to 36 healthy volunteers. These people take both the brand-name drug and the generic, in random order, on an empty stomach. Blood samples are taken over hours to map how the drug moves through the body. The results are compared statistically. If the confidence interval for AUC and Cmax falls within 80-125%, the drug passes.For complex products - like inhalers, nasal sprays, or topical creams - testing gets trickier. You can’t just draw blood and measure concentration. Instead, manufacturers might use in vitro tests, clinical endpoint studies, or even measure how well the drug reduces symptoms. The FDA has issued over 25 guidance documents since 2020 to help companies prove bioequivalence for these harder-to-measure drugs.
Cost savings and global differences
The whole system exists to save money - and it works. Generic drugs save patients an average of $313 per prescription. Over the past decade, they’ve saved the U.S. healthcare system an estimated $2.2 trillion. That’s why 90% of prescriptions are generics. But the rules aren’t the same everywhere. The European Medicines Agency (EMA) allows wider ranges - up to 75-133% - for drugs that behave unpredictably in the body. The FDA doesn’t accept that. It sticks to tighter limits, especially for drugs with narrow therapeutic windows.Some countries also require testing under both fed and fasted conditions. The U.S. usually only requires one. That’s why a generic made in India and approved in Europe might not be approved in the U.S. - not because it’s unsafe, but because it doesn’t meet the stricter U.S. bioequivalence standards.

What patients really experience
Surveys show most people are happy with generics. A 2023 Consumer Reports survey found 78% of users were satisfied with generic medications, compared to 82% for brand names. The biggest gap? Antiepileptic drugs - where 12% more people reported issues with generics. That’s why many states require pharmacists to keep you on the same generic brand once you’ve started. If you feel different after a switch - whether it’s more side effects, less effectiveness, or just a weird feeling - talk to your doctor. It’s not common, but it happens.And while online forums like Reddit sometimes buzz with stories of “my generic didn’t work,” the data doesn’t back up widespread problems. The FDA’s adverse event database shows only 0.3% of all medication reports involve generics - which matches their market share. That’s not a coincidence. It’s proof the system works.
What’s changing now
The FDA is investing $25 million through 2027 to improve bioequivalence methods for complex drugs. New tools like pharmacometric modeling - which uses computer simulations to predict how a drug behaves in different people - might one day replace fixed 80-125% ranges. Instead of one-size-fits-all limits, we might see personalized thresholds based on your genetics, age, or liver function. That’s still years away. But it shows regulators know the system isn’t perfect.For now, the current standards are reliable. For the vast majority of drugs - antibiotics, blood pressure pills, antidepressants, statins - bioequivalence means you can trust the generic. You’re getting the same medicine. Just cheaper.
What to do if you’re unsure
If you’ve been switched to a generic and feel something’s off:- Check the drug’s therapeutic equivalence code in the FDA’s Orange Book (searchable online).
- Ask your pharmacist which generic manufacturer you’re getting. Stick with the same one if possible.
- Keep a symptom log: when did you start the new pill? Did headaches, dizziness, or mood changes start then?
- Talk to your doctor. Don’t assume it’s “all in your head.”
Most of the time, the generic will work fine. But if it doesn’t, you have options. Your doctor can prescribe the brand name, or ask for a specific generic manufacturer. You’re not stuck with whatever the pharmacy sends.