When you feel a sharp, constant pain in your lower left abdomen, along with fever and nausea, it’s easy to assume it’s just a bad stomach bug. But if you’re over 50 - or even in your 30s or 40s these days - that pain could be something more specific: diverticulitis. It’s not just a passing discomfort. It’s inflammation in small pouches that form in your colon wall, and if ignored, it can lead to serious complications.
What Exactly Are Diverticula?
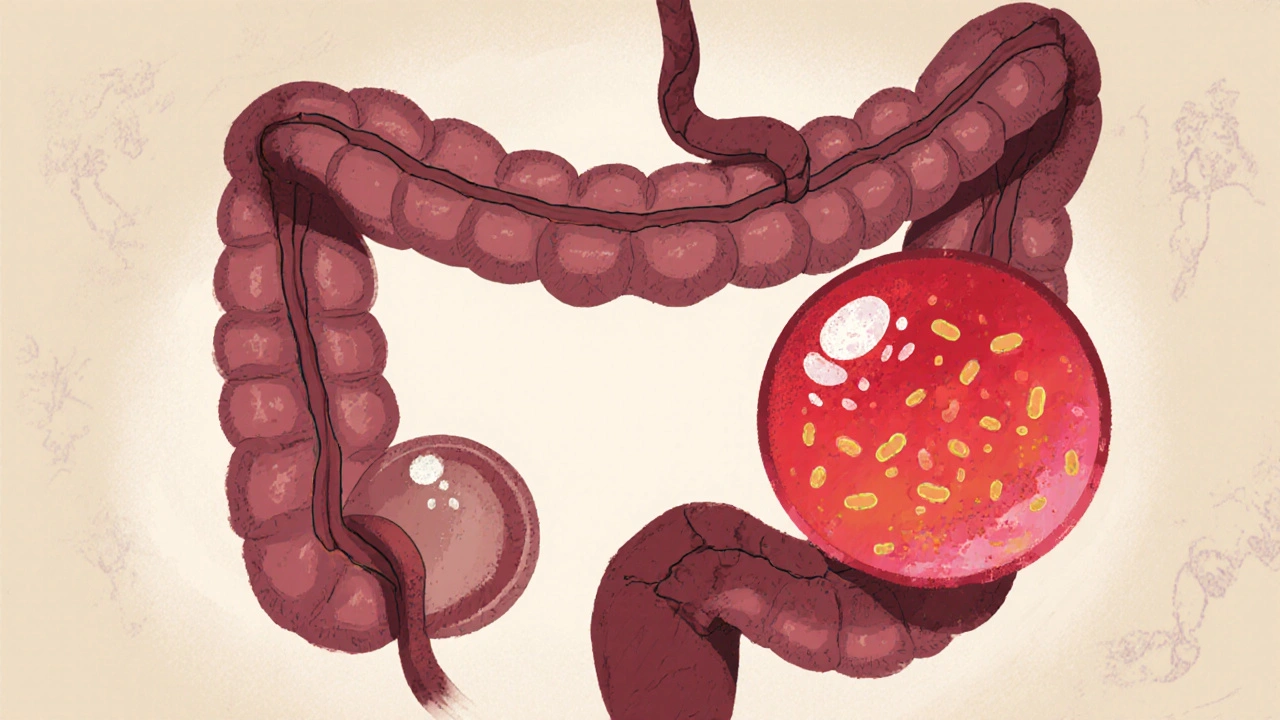
Diverticula are tiny, balloon-like sacs that stick out from the colon. They’re not cancerous, and they don’t always cause problems. In fact, about 35% of Americans under 50 have them, and by age 60, that number jumps to nearly 60%. This condition, called diverticulosis, is so common it’s often found by accident during a routine colonoscopy or CT scan. But when one of these pouches gets blocked by stool or bacteria, it can become inflamed - that’s diverticulitis.The sigmoid colon, the last part of the large intestine before the rectum, is where 95% of these pouches form. That’s why the pain is usually on the lower left side. But in Asian populations, it’s more common on the right side, thanks to differences in colon anatomy. The pouches themselves are small - about 5 to 10 millimeters - but when they swell, they can cause real damage.
How Do You Know It’s Diverticulitis and Not Something Else?
Many people mistake diverticulitis for irritable bowel syndrome (IBS), appendicitis, or even ovarian cysts. But there are clear differences. IBS brings cramps that come and go, often tied to meals or stress. Diverticulitis pain is steady, sharp, and often gets worse when you move. You’re also more likely to have a fever - over 38°C (100.4°F) - which happens in 70 to 80% of cases. Blood tests often show elevated white blood cells, meaning your body is fighting an infection.Doctors rely on a CT scan to confirm the diagnosis. It shows not just the inflamed pouches, but also whether there’s an abscess, a hole, or spreading infection. Without imaging, up to 25% of cases get misdiagnosed. One patient I read about visited three doctors over five days before getting the right answer. That delay isn’t unusual. On average, people wait over three days to get diagnosed properly.
How Bad Is It? The Hinchey Scale Explained
Not all cases are the same. Doctors use the Hinchey classification to grade severity:- Stage Ia: Small abscess around the colon (less than 3 cm)
- Stage Ib: Larger abscess (3-5 cm) or more widespread inflammation
- Stage II: Abscess in the pelvis
- Stage III: Generalized pus in the abdomen
- Stage IV: Fecal matter leaks into the abdomen - a medical emergency
Most cases (about 75%) are Stage I or II and can be treated without surgery. But if you’re in Stage III or IV, you need immediate hospital care - and possibly surgery.
What’s the Best Treatment Today?
The biggest change in diverticulitis care happened in the last five years. For decades, antibiotics were given to everyone. Now, that’s no longer the case.A major 2021 study called the DIVERT trial showed that for mild, uncomplicated diverticulitis, antibiotics didn’t speed up recovery. Patients given only rest, fluids, and pain relief did just as well as those on antibiotics. Today, guidelines from the American Gastroenterological Association say: if you’re otherwise healthy, have no fever, and your CT scan shows only mild inflammation, skip the antibiotics.
But if you have a fever over 38.5°C, a high white blood cell count, or you’re elderly or immunocompromised, antibiotics are still necessary. Common choices include amoxicillin-clavulanate (875/125 mg twice daily) or a combination like piperacillin-tazobactam if you’re in the hospital.
Pain relief is tricky. Avoid ibuprofen, naproxen, or other NSAIDs - they increase the risk of a tear in the colon. Stick with acetaminophen (paracetamol), 500-1,000 mg every 6 hours as needed.

Diet: What to Eat (and What Not to Fear)
For years, doctors told people with diverticulitis to avoid nuts, seeds, popcorn, and corn. That advice came from old assumptions that these foods could get stuck in the pouches and cause inflammation. But a massive 18-year study of 47,000 women - the Nurses’ Health Study - found no link at all. In fact, those who ate more nuts and seeds had lower rates of diverticulitis.During an active flare-up, you’ll start with a clear liquid diet: water, broth, gelatin, and apple juice. After 48-72 hours, you’ll move to low-fiber foods like white rice, eggs, and canned vegetables without skins. Once symptoms ease, you gradually increase fiber - aiming for 25-35 grams daily. That means whole grains, beans, lentils, fruits, and vegetables. Fiber keeps stool soft and reduces pressure in the colon, which helps prevent new pouches from forming - or old ones from getting inflamed again.
One patient on a health forum said after his second attack, he upped his fiber to 35 grams a day and hasn’t had another flare-up in over two years.
When Surgery Might Be Needed
Most people never need surgery. But if you’ve had two or more attacks that required hospitalization, your doctor might talk about removing the affected part of the colon. The old rule was three attacks. Now, it’s two - especially if your quality of life is suffering between episodes.For complicated cases, two main procedures exist:
- Laparoscopic lavage: Wash out the infection without removing the colon. Works well for contained perforations, with an 82% success rate.
- Resection: Remove the diseased section. Often done if there’s a large abscess or recurrent disease.
A 2022 trial called SCANDIV showed laparoscopic lavage was just as safe as removal for many patients - and meant shorter hospital stays.
What Happens After the Flare-Up?
Once the inflammation clears, you’ll usually get a colonoscopy 6 to 8 weeks later. Why? Because diverticulitis symptoms can mimic colon cancer. A 2021 JAMA study found that 1.3% of patients over 50 had hidden cancer when they had their first diverticulitis episode. That’s low, but not negligible - and catching it early saves lives.
Who’s at Risk?
Diverticulitis used to be seen as an older adult’s disease. Now, it’s rising fast in younger people. In 2000, only 14% of hospitalizations were in people under 44. Today, it’s 22%. Why?- Obesity: BMI over 30 doubles your risk.
- Smoking: Smokers are nearly three times more likely to develop it.
- Sedentary lifestyle: People who exercise less than two hours a week have a 38% higher chance.
- Low-fiber diet: Even if you’re young, eating processed foods and skipping vegetables raises your risk.
And while genetics play a role, lifestyle is the biggest driver. That means you have more control than you think.
New Hope: Medications and AI
Preventing recurrence is the new frontier. A drug called mesalazine (Pentasa®), used for years for ulcerative colitis, was recently approved in the U.S. for diverticulitis maintenance. In a 2023 trial, it cut recurrence rates by 31% over a year compared to placebo.Meanwhile, AI is stepping in. Mayo Clinic developed a tool that looks at your CT scan, blood results, age, and BMI to predict your chance of another attack - with 83% accuracy. That helps doctors decide who needs closer follow-up or preventive therapy.
Researchers are also studying the gut microbiome. People with diverticulitis often have lower levels of Faecalibacterium prausnitzii - a beneficial bacterium that helps calm inflammation. Future treatments may involve targeted probiotics or fecal transplants.
Bottom Line: You Can Manage This
Diverticulitis isn’t a death sentence. It’s not even always a lifelong battle. For most people, it’s a one-time event - or maybe two - that can be handled with diet, rest, and smart medical choices. The key is not to panic when symptoms start, but to act quickly and correctly.Don’t delay seeing a doctor if you have persistent left-sided pain and fever. Don’t fear nuts or seeds - they’re safe. Don’t skip your follow-up colonoscopy. And don’t assume antibiotics are always needed. The best treatment today isn’t just medicine - it’s knowledge, diet, and listening to your body.
Can diverticulitis go away on its own?
Yes, mild cases of diverticulitis can resolve without antibiotics or surgery. With rest, hydration, and a clear liquid diet followed by a gradual return to high-fiber foods, many people recover fully within a week. Studies show that for uncomplicated cases, the body can clear the inflammation on its own. But you still need a doctor to confirm it’s not something more serious.
Is diverticulitis the same as diverticulosis?
No. Diverticulosis means you have pouches in your colon but no inflammation or symptoms. It’s common and often harmless. Diverticulitis happens when one or more of those pouches become infected or inflamed, causing pain, fever, and other symptoms. Think of diverticulosis as the condition, and diverticulitis as the complication.
Why can’t I take ibuprofen for the pain?
NSAIDs like ibuprofen and naproxen can increase the risk of a tear or hole in your colon wall, especially when it’s already inflamed. Even if the pain feels like a regular headache, it’s safer to use acetaminophen (paracetamol) instead. It doesn’t affect the gut lining and still gives you effective pain relief.
Should I avoid fiber during a flare-up?
Yes - temporarily. During an active flare, high-fiber foods can make bloating and cramping worse. Stick to low-fiber options like white bread, eggs, and cooked vegetables without skins. Once symptoms improve over a few days, slowly reintroduce fiber. Long-term, high fiber is your best defense against recurrence.
Do I need surgery after multiple attacks?
Not automatically. Surgery is now considered after two attacks that required hospitalization, especially if you’re having ongoing pain or reduced quality of life between episodes. For many, managing diet and lifestyle is enough. But if you’ve had complications like abscesses or perforations, surgery may be the safer long-term choice.
Can I still eat nuts and seeds?
Absolutely. Older advice to avoid nuts, seeds, and popcorn has been completely debunked. A 18-year study of 47,000 women found no link between eating these foods and increased diverticulitis risk. In fact, those who ate more nuts had lower rates of flare-ups. They’re part of a healthy, high-fiber diet.
How can I prevent diverticulitis from coming back?
Focus on three things: eat 25-35 grams of fiber daily from whole grains, beans, fruits, and vegetables; stay physically active (at least 150 minutes a week); and avoid smoking. If you’ve had more than one episode, talk to your doctor about mesalazine, which can reduce recurrence by over 30%. Regular colonoscopies after an attack also help catch other issues early.

Erika Sta. Maria
Okay but have you ever considered that diverticulitis is just capitalism’s way of punishing you for eating too many organic kale chips? I mean, colon pouches? That’s what happens when your body rebels against the grind. We’re not broken-we’re *resisting*. Also, I think I had it last Tuesday but I just drank chamomile tea and yelled at my Wi-Fi router. It went away. Coincidence? I think not.
Nikhil Purohit
Man, this post is gold. I had my first flare-up last year at 31-thought it was food poisoning. Turns out I was eating like a college student who thinks ‘fiber’ is a type of yoga. Started eating lentils and flax, hit the gym 3x a week, and no more drama. No antibiotics needed. Seriously, if you’re under 40 and getting this, check your diet before your meds.
Debanjan Banerjee
Let’s correct a few inaccuracies in the original post. First, the DIVERT trial was not the first to challenge antibiotic use-multiple RCTs since 2017 (including the Dutch DIABOLO trial) had already shown non-inferiority of conservative management. Second, mesalazine’s efficacy in diverticulitis is still controversial-only one small RCT showed marginal benefit, and it was industry-funded. Third, the 1.3% cancer rate in JAMA was from a retrospective cohort, not prospective screening. Don’t treat this as gospel-evidence evolves. And yes, you can still take NSAIDs if you’re low-risk and monitored. Context matters.
Steve Harris
Thank you for this incredibly clear breakdown. As a nurse practitioner, I see too many patients terrified of nuts or convinced they need antibiotics for every twinge. This post nails the modern approach: listen to the body, trust the data, avoid fear-based advice. I’ve started handing out printed summaries of this to my patients. If you’re reading this and have diverticulosis-don’t panic. Eat your beans. Move your body. And yes, you’re allowed to eat popcorn.
Cooper Long
Diverticulitis is not a disease of the colon. It is a disease of modernity. The human gut evolved over millennia to process coarse, fibrous vegetation under conditions of intermittent fasting and constant physical exertion. We now consume refined carbohydrates, sit for 12 hours a day, and ingest synthetic additives. The colon, a noble organ, has no choice but to rebel. The pouches are not defects-they are warnings. The real question is not how to treat the inflammation, but how to restore the ecological balance our ancestors knew.
Sheldon Bazinga
bro i got diverticulitis in 2021 and i swear it was the fbi putting something in my protein powder. i mean why else would it hit me right after i started using that ‘plant-based’ stuff? also why do all the doctors say ‘fiber’ like its magic? i think they’re paid by the oat bran lobby. i stopped eating everything and now i just drink bone broth and stare at the wall. it worked. 10/10 recommend. also i saw a guy on tiktok say the colon is a portal. i believe him.
Sandi Moon
Let me ask you this: Who benefits from the narrative that diverticulitis is ‘common’ and ‘manageable’? The pharmaceutical industry? The hospital chains? The ‘fiber’ conglomerates? The fact that 95% of pouches form in the sigmoid colon? That’s not anatomical coincidence-it’s engineered. The same corporations that sell you processed foods also sell you the ‘solution’-fiber supplements, colonoscopies, and now, mesalazine. This is not medicine. This is control. And yes, I’ve seen the data. I’ve seen the funding. And I know what’s really going on.
Kartik Singhal
bro i had 3 flare-ups in 2 years and now i just eat 10 almonds every morning and cry into my matcha latte 🥲 the docs told me to eat fiber but i’m like ‘what if the fiber is the problem?’ also i read somewhere that diverticulitis is just your colon’s way of saying ‘i miss the 1800s’ 🤔 so now i only eat raw meat and stare at the moon. it’s working. also i got a tattoo that says ‘diverticula > capitalism’ 🖤
Logan Romine
So let me get this straight. We’ve spent 50 years telling people to avoid nuts… then suddenly it’s ‘actually, nuts are great’? And now we’re telling people antibiotics are useless… but only if you’re young, healthy, and have a CT scan that looks like a Pinterest board? Meanwhile, the guy who ate a bag of popcorn and got sepsis? Nah, he’s just ‘not statistically significant.’ 😏 We don’t need more ‘guidelines.’ We need less arrogance disguised as science.