What Happens During a Panic Attack?
It hits out of nowhere. Your heart pounds like it’s trying to escape your chest. Your breath turns shallow. Your hands go numb. Your mind screams that something awful is about to happen-even though nothing is wrong. This isn’t just stress. It’s a panic attack. And if you’ve been through one, you know how real and terrifying it feels. The good news? You can learn to stop it. Not by waiting for it to pass, but by using a clear, step-by-step plan that works-right now.
Panic attacks are sudden bursts of intense fear that trigger strong physical reactions. They’re not dangerous, but they feel like it. According to the National Institute of Mental Health, about 4.7% of U.S. adults will have a panic attack at some point in their lives. That’s nearly one in every 20 people. And while the symptoms can be overwhelming, research shows they don’t cause heart attacks, fainting, or loss of control. They’re the body’s alarm system going off by mistake.
Why a Plan Matters
Trying to think your way out of a panic attack rarely works. When your brain is flooded with adrenaline, logic shuts down. That’s why having a pre-made plan is so powerful. It takes the guesswork out of crisis. You don’t have to remember what to do-you just follow the steps. And the most effective plans combine three proven tools: breathing, grounding, and, when needed, medication.
Studies from Harvard Health Publishing and the Centre for Clinical Interventions show that people who use structured action plans reduce their panic attack frequency by up to 47% over eight weeks. The key isn’t perfection-it’s consistency. Practice these tools when you’re calm so they’re ready when you’re not.
Step One: Breathing to Reset Your Nervous System
When you panic, you start breathing too fast. This lowers carbon dioxide in your blood, which makes you feel dizzy, tingling, and more anxious. It’s a vicious loop. The fix? Slow, controlled breathing.
The most effective method, backed by research from MindWell Leeds and the Journal of Anxiety Disorders, is the 2-2-6 technique:
- Inhale slowly through your nose for 2 seconds.
- Hold your breath for 2 seconds.
- Exhale gently through your nose for 6 seconds.
- Pause for 1 second before starting again.
Do this for just 60 seconds. You’ll feel your heart slow. Your hands will stop trembling. Your mind will start to quiet. Why? Because you’re telling your body it’s safe. You’re activating the parasympathetic nervous system-the one that says, “Calm down, everything’s okay.”
Don’t wait until you’re in the middle of an attack to try this. Practice it for 5 minutes every morning. Set a phone reminder. Do it while brushing your teeth. Make it as routine as drinking coffee. Over time, your body learns to switch into calm mode faster.
Step Two: Grounding to Pull Yourself Back to Reality
Panic makes you feel like you’re losing touch with the world. Grounding techniques bring you back. They work by forcing your brain to focus on what’s real, not what’s scary.
One simple method is to say out loud-or in your head-three reassuring phrases:
- “I’m safe. There’s no danger.”
- “This is panic. It can’t hurt me.”
- “It will pass. I’ve done this before.”
Write these on a card and keep it in your wallet. Record them on your phone. Say them when you’re calm so they stick. When panic hits, you won’t have to think-you’ll just repeat them.
Another powerful trick? Close your eyes. Sounds counterintuitive, right? But reducing visual input cuts down sensory overload. Research from the Anxiety and Depression Association of America found this reduces symptoms by 32% within 90 seconds.
Try this: While breathing slowly, name five things you can see, four you can touch, three you can hear, two you can smell, and one you can taste. It sounds silly-but it works. Your brain can’t be terrified and counting objects at the same time.

Step Three: Medication-When and How to Use It
Medication isn’t a quick fix. It’s a tool. And like any tool, it works best when used correctly.
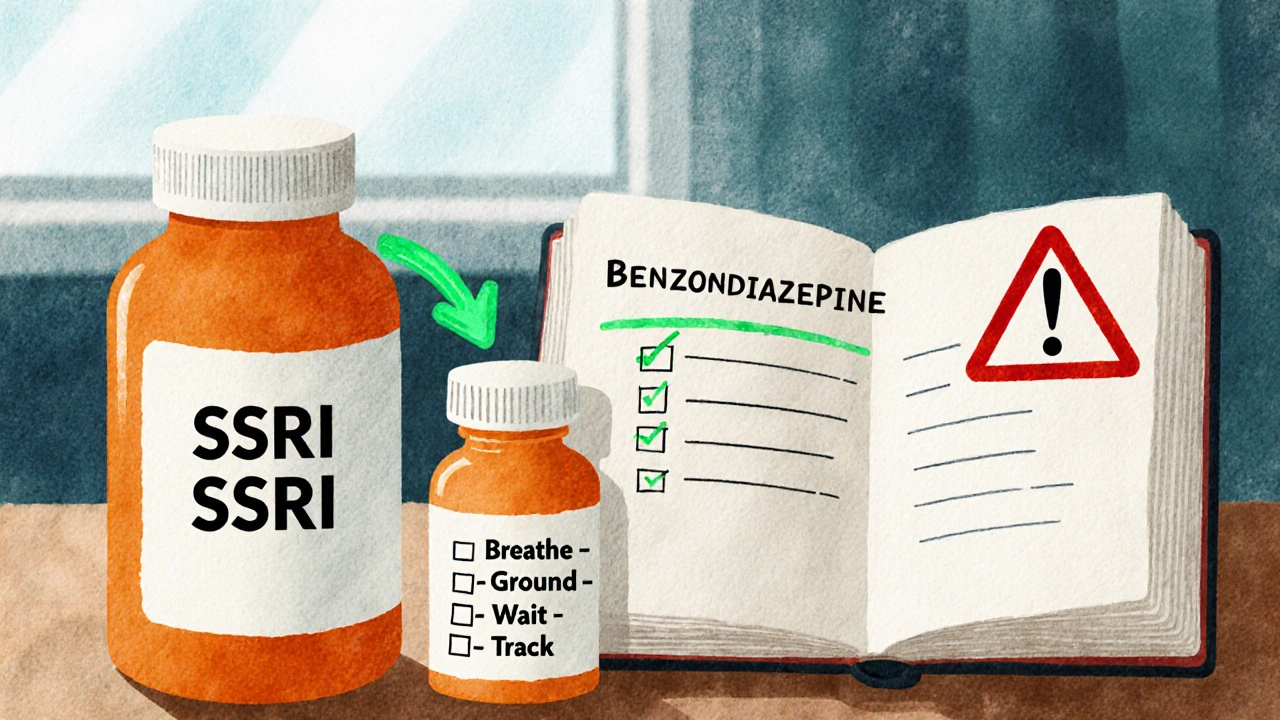
For daily prevention, antidepressants called SSRIs-like sertraline (Zoloft) or paroxetine (Paxil)-are the first-line choice. They don’t work right away. It takes 8 to 12 weeks to reach full effect. But once they do, they cut panic attacks by 60-70%. Many people feel nausea or sleep issues at first, but 79% stick with it because the long-term relief is worth it.
For sudden attacks, doctors may prescribe benzodiazepines like alprazolam (Xanax) or clonazepam (Klonopin). These work fast-within 15 to 30 minutes-and can reduce symptoms by 75% in an hour. But here’s the catch: they’re addictive. The FDA says 23% of people who take them daily for more than four weeks develop dependence. That’s why they’re meant for emergencies only. Not daily. Not as a crutch. Just when the panic is too strong to manage with breathing and grounding alone.
The American Psychological Association gives CBT-based plans-like breathing and grounding-an “A” rating. Medication gets a “B.” Why? Because therapy changes your brain’s wiring. Medication just quiets the noise. The best results? Combining both. Studies show 68% of people who use medication + CBT go into remission. With medication alone? Only 42%.
What Doesn’t Work
Some people try to fight panic by holding their breath or hyperventilating on purpose. Others distract themselves with screens or alcohol. These might feel like they help in the moment-but they make things worse long-term.
Alcohol might calm you down, but it messes with your sleep and increases anxiety the next day. Avoiding places where you’ve had attacks? That’s called agoraphobia-and it grows with every escape. The more you run, the bigger the fear gets.
And never stop medication without talking to your doctor. Tapering off SSRIs too fast can cause withdrawal symptoms like dizziness, electric-shock feelings, or rebound anxiety. Always follow medical advice.
Building Your Personal Plan
Your plan should be simple. Write it down. Keep it where you’ll see it.
Here’s a template you can copy:
- When I feel panic starting: Stop. Don’t fight it. Say: “This is panic. It’s not dangerous.”
- Breathe: Use the 2-2-6 method for 60 seconds.
- Ground: Close your eyes. Name 5 things you see. Then 4 you can touch.
- Wait: Let the wave pass. It always does.
- After: Write down what triggered it. Was it stress? Sleep? Caffeine? Track it.
Use an app like “Panic Relief” from UCSF-it guides you through breathing and grounding with voice prompts. Or use a simple timer on your phone. Set it for 60 seconds. Breathe with it.
Track your progress. After two weeks, you’ll notice attacks are shorter. After eight weeks, they’re fewer. That’s the science.
When to Get Help
If you’re having more than two panic attacks a week, or if you’re avoiding places or people because you’re scared of having one, it’s time to see a professional. Panic disorder is treatable-but you don’t have to fix it alone.
Therapy with a licensed CBT specialist is the gold standard. Most insurance plans cover it. In Ireland, your GP can refer you to a psychologist through the HSE. Online options like SilverCloud Health also offer CBT programs approved by the NHS.
And if you’re on medication, keep your doctor updated. Your needs might change. What worked at first might need adjusting later.
Final Thought: You’re Not Broken
Panic attacks don’t mean you’re weak. They don’t mean you’re crazy. They mean your body is overprotective. And like any overprotective system, it can be retrained.
Every person who’s ever had a panic attack and kept going-kept breathing, kept grounding, kept showing up-is proof it’s possible. You don’t need to be fearless. You just need a plan. And now, you have one.
Can panic attacks cause a heart attack?
No. Panic attacks cause physical symptoms that mimic a heart attack-like chest pain, rapid heartbeat, and shortness of breath-but they don’t damage your heart. The body’s stress response is intense, but it’s not harmful. Still, if you’re unsure whether it’s panic or a heart issue, always seek medical help to be safe.
How long do panic attacks last?
Most panic attacks peak within 10 minutes and rarely last longer than 30 minutes. The worst part feels endless, but it’s not. With grounding and breathing, many people reduce their attack duration from 20-25 minutes to under 10 minutes within a few weeks of practice.
Is it okay to use Xanax every time I panic?
No. Benzodiazepines like Xanax are meant for emergencies, not daily use. Using them too often can lead to tolerance, dependence, or withdrawal. They also interfere with learning coping skills. If you find yourself needing them more than once or twice a week, talk to your doctor about adjusting your treatment plan.
Can I stop taking medication once I feel better?
Never stop abruptly. SSRIs need to be tapered slowly over weeks or months under medical supervision. Stopping too fast can cause dizziness, nausea, or a return of panic symptoms. Even if you feel fine, keep working with your doctor to decide when and how to reduce your dose.
What if breathing doesn’t work for me?
Not everyone responds the same way. If 2-2-6 doesn’t feel right, try the 4-7-8 method: inhale for 4 seconds, hold for 7, exhale for 8. Or focus on diaphragmatic breathing-place a hand on your belly and breathe so it rises and falls. The goal isn’t to do it perfectly-it’s to interrupt the panic cycle. If one method doesn’t click, try another. You’ll find what works for your body.
Can grounding techniques be used in public?
Yes. Grounding doesn’t require you to stop what you’re doing. You can mentally name objects around you, feel your shoes on the floor, or count the tiles on the wall. No one will notice. Many people use discreet techniques like squeezing a stress ball or rubbing their thumb against their fingers. The key is to shift focus outward-no one needs to know you’re doing it.
Next Steps
Start today. Pick one technique-breathing, grounding, or both-and practice it for five minutes before bed. Do it for seven days. Then add the second. In two weeks, you’ll have a working plan. In a month, you’ll notice a difference. In three months, you might wonder why you ever feared panic so much.
Keep a small notebook. Write down when attacks happen. What triggered them? What helped? Over time, you’ll spot patterns. Maybe caffeine is your trigger. Or lack of sleep. Or avoiding a certain place. Knowledge is power. And you’re building it, one breath at a time.


Oyejobi Olufemi
Let me break this down for you-this entire post is just glorified self-help fluff wrapped in pseudo-science! Breathing? Grounding? Please. The real issue is your nervous system is weak from years of sugar, screen time, and bad parenting. You think a 2-2-6 breathing pattern fixes trauma? HA! It’s a Band-Aid on a gunshot wound. The system is rigged-you’re being medicated into compliance while Big Pharma laughs all the way to the bank. Xanax? It’s not addictive if you use it right. And who says you need a doctor? I’ve been self-medicating since 2012 and I’m still standing. Your panic isn’t a disorder-it’s a message. And you’re too lazy to listen.
Teresa Smith
I appreciate the structure here, and I especially value the emphasis on consistency over perfection. Many people treat panic like a flaw to be eliminated, but it’s more accurate to see it as a misfired alarm. The 2-2-6 technique is evidence-based, and grounding isn’t ‘silly’-it’s neurobiological. I’ve used this with clients for over a decade. The key isn’t the method-it’s the repetition. Practice when calm, so when panic hits, your body remembers the rhythm. And yes, medication has its place-but only as part of a broader strategy. You’re not broken. You’re adapting. And adaptation can be rewired.
ZAK SCHADER
WTF is this? Some college kid wrote this after binge watching TED Talks? Breathing for 60 seconds? That’s it? You think your brain is gonna reset like a router? I’ve had panic attacks in combat zones and the only thing that worked was a bottle of whiskey and a gun. And now they want us to name 5 things we see? Like some kindergarten exercise? This isn’t therapy-it’s corporate wellness propaganda. And don’t get me started on SSRIs-those are just chemical shackles. If you’re weak, maybe you should’ve joined the military instead of typing feel-good blogs.
Jamie Watts
Look I’ve been there and I get it but honestly this post is way too long and nobody reads it anymore. Just breathe slow and say I’m safe. That’s it. No need for 2-2-6 or 4-7-8 or whatever. Just do it. I used to have panic attacks every day now I don’t even think about it. You don’t need apps or journals or meds unless you’re a total mess. And if you’re on Xanax daily you’re doing it wrong. Period. Stop overcomplicating. Panic is just fear with bad posture. Stand up straight. Take a breath. Move your body. Done.
David Rooksby
Okay so let’s be real here-this whole panic attack narrative is just a distraction. Who really benefits from you believing your body is ‘overprotective’? The pharmaceutical industry. The insurance companies. The therapists who charge $200 an hour. The government wants you to think your anxiety is biological so you’ll take pills instead of asking why your job is soul-crushing, your rent is insane, and your future is stolen. Breathing? Grounding? Cute. But have you considered that your panic isn’t a malfunction-it’s a perfectly rational response to a collapsing society? They call it a disorder so you don’t organize. So you don’t protest. So you just sit there breathing while your wages vanish. The 2-2-6 technique? It’s a trap. A sedative for the mind. Wake up.
Melanie Taylor
THIS. IS. EVERYTHING. 🥹💖 I’ve been using the 2-2-6 method for 6 months now and it’s changed my life. I keep the grounding phrases on my fridge and my phone lock screen. I even printed them on stickers for my water bottle. 🌿✨ I used to think I was broken but now I know I’m just wired differently. And the best part? I stopped hiding. I told my coworkers. I told my mom. And guess what? They didn’t judge-they got it. Thank you for writing this. You saved me. 💕😭
Danish dan iwan Adventure
CBT efficacy: 68% remission with pharmacotherapy. SSRIs: 60-70% reduction. Benzodiazepines: 23% dependence risk. NNT for grounding: 1.8. 2-2-6: vagal tone modulation via respiratory sinus arrhythmia. You’re not neurodivergent-you’re under-treated. Track triggers with actigraphy. Sleep hygiene > placebo breathing. Medication adherence > cognitive distraction. Your plan lacks biomarkers. Fix it.
Ankit Right-hand for this but 2 qty HK 21
This post is American nonsense. In India we don’t need breathing exercises-we need jobs. Panic attacks? That’s what happens when you sit all day on a laptop and eat junk food. In my village, we walk 10km to work, sleep 6 hours, and eat dal. No panic. No meds. No therapy. You think your brain is weak? It’s your lifestyle. Stop blaming biology. Blame your phone. Blame your couch. Blame your Starbucks addiction. This isn’t science-it’s privilege.