Most people think hemorrhoids are just a minor annoyance-something you get from sitting too long or eating too little fiber. But if you’ve had one, you know it’s more than that. It’s the burning after a bowel movement. The lump you can’t ignore. The fear that every streak of blood means something worse. And here’s the truth: hemorrhoids are far more common than you think. About 75% of people will deal with them at some point in their lives. The good news? Most don’t need surgery. The better news? You can tell the difference between internal and external hemorrhoids-and treat them properly-if you know what to look for.
What Exactly Are Hemorrhoids?
Hemorrhoids aren’t a disease. They’re normal blood vessels-like cushions-that help you control bowel movements. Think of them like shock absorbers inside your anus. But when pressure builds up-because of constipation, pregnancy, heavy lifting, or sitting too long-they swell. That’s when they become a problem. There are two main types: internal and external. They’re not just different in location-they’re different in how they feel, what they do, and how you treat them. And yes, you can have both at the same time. That’s why so many people get confused.Internal Hemorrhoids: Silent but Not Harmless
Internal hemorrhoids form inside the rectum, above a line called the dentate line. This area has no pain nerves, so even when they’re swollen, you often won’t feel pain. That’s why they’re sneaky. The main sign? Bright red blood. You might see it on the toilet paper, in the bowl, or on your stool. It’s usually painless. Sometimes, you’ll feel like you haven’t fully emptied your bowels, or you’ll feel pressure deep inside. That’s the internal hemorrhoid pushing down. Doctors grade them from I to IV:- Grade I: Bleeds, but doesn’t bulge out.
- Grade II: Pops out when you strain, but goes back in on its own.
- Grade III: Comes out and you have to push it back in.
- Grade IV: Stays out all the time. Can’t be pushed back. This one often needs treatment.
External Hemorrhoids: Pain You Can’t Ignore
External hemorrhoids form under the skin around your anus. This area is packed with nerves. So when they swell? You feel it. Symptoms are harder to miss:- A tender lump you can see or feel
- Itching or irritation around the anus
- Pain that gets worse when you sit
- Swelling that feels like a balloon
Why You Might Be Mistaking It for Something Else
A lot of people think every itch, bleed, or lump is a hemorrhoid. But that’s dangerous. An anal fissure-a small tear in the lining of the anus-also causes bleeding and pain. But here’s the difference: fissures cause a sharp, tearing pain during bowel movements. Hemorrhoids cause more of a dull ache, pressure, or burning after. Fissures rarely cause lumps. Hemorrhoids do. And here’s the big one: rectal bleeding isn’t always hemorrhoids. Colorectal cancer, inflammatory bowel disease, or infections can look the same. If you’re over 50, have a family history of colon cancer, or notice changes in your bowel habits (like new constipation or diarrhea), don’t assume it’s just hemorrhoids. Get checked.
What You Can Do at Home
For mild cases, you don’t need a doctor right away. Start here:- Eat more fiber. Aim for 25-30 grams a day. That’s 2 cups of beans, 1 cup of oats, 2 apples, and a handful of almonds. Fiber softens stool so you don’t have to strain.
- Drink water. At least 8 glasses a day. Fiber without water makes constipation worse.
- Use a footstool. Put your feet up while you sit on the toilet. This positions your body to push naturally, reducing pressure on your rectal veins by about 30%.
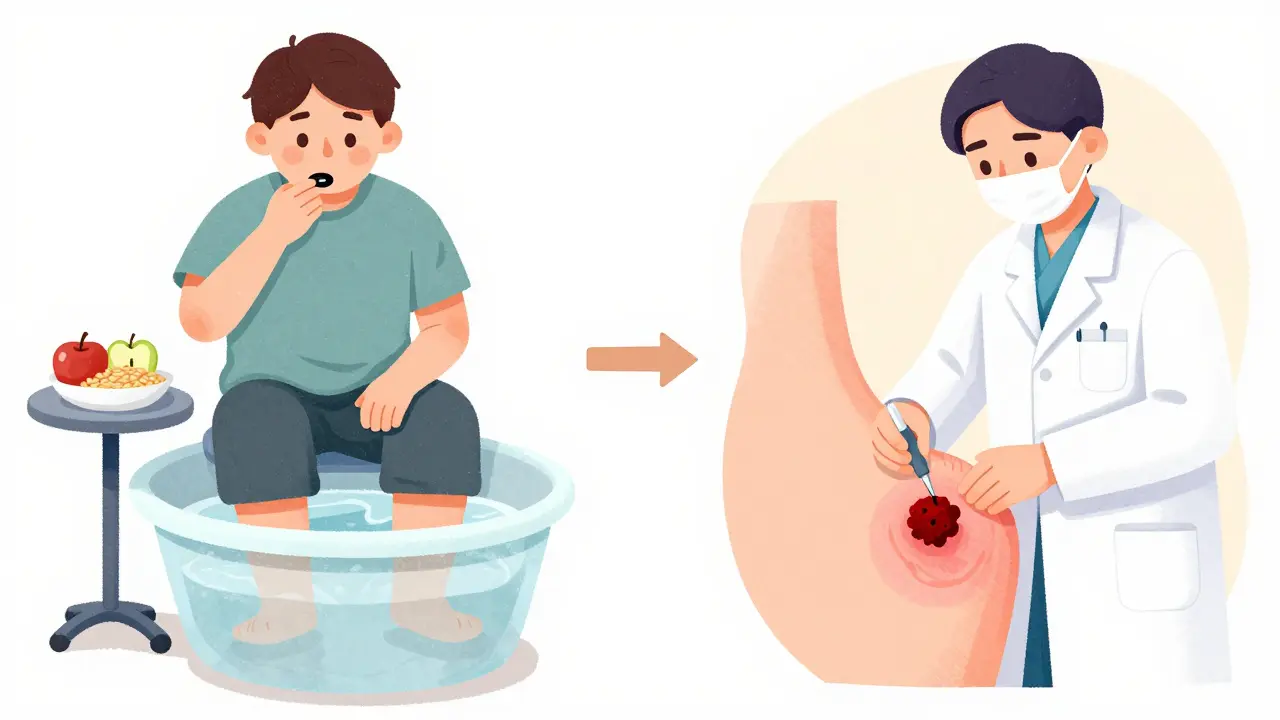
- Take sitz baths. Sit in warm water for 15 minutes, 2-3 times a day. It reduces swelling and soothes irritation.
- Avoid sitting too long. Don’t read or scroll on your phone on the toilet. Five minutes max.
- Use over-the-counter creams. Hydrocortisone helps with itching. Witch hazel pads reduce swelling. Don’t use them for more than a week without checking with a doctor.
When Home Care Isn’t Enough
If your hemorrhoids keep coming back or won’t go away after a few weeks, it’s time for medical help. For internal hemorrhoids, doctors have three common office procedures:- Rubber band ligation: A tiny band is placed around the base of the hemorrhoid. It cuts off blood flow. The hemorrhoid shrivels and falls off in a few days. It’s 90% effective for Grades I-III. You might feel pressure or mild cramping for a day or two.
- Sclerotherapy: A chemical is injected into the hemorrhoid. It causes scarring and shrinkage. Less effective than banding, but good for people who can’t tolerate banding.
- Infrared coagulation: A brief burst of heat seals the blood vessels. You feel a quick zap. No anesthesia needed. Good for smaller hemorrhoids.
Surgery: The Last Resort
If you have Grade IV hemorrhoids, recurrent problems, or failed other treatments, surgery might be needed.- Hemorrhoidectomy: The hemorrhoid is completely cut out. It’s the most effective-95% success rate. But recovery takes 2-4 weeks. Pain is real. You’ll need painkillers. It’s not fun, but it’s permanent.
- Stapled hemorrhoidopexy: Instead of removing the hemorrhoid, the doctor staples it back up inside. Less pain than a traditional cut-out, but higher chance of recurrence. Often used for prolapsed hemorrhoids.
Prevention Is the Real Treatment
Hemorrhoids come back if you don’t change your habits. Studies show that people who stick to high-fiber diets, drink enough water, and avoid straining have only a 5-10% chance of recurrence. Those who don’t? Up to 50%. For pregnant women-who are 25-35% more likely to get hemorrhoids-sleeping on your left side and doing pelvic floor exercises can help reduce pressure. And skip the miracle cures online. No oil, no herb, no cream sold as a “cure-all” has proven results. Stick to what science backs: fiber, water, movement, and proper toilet habits.When to See a Doctor
You don’t need to suffer in silence. Call a doctor if:- Bleeding lasts more than a week
- Pain is severe or getting worse
- You feel dizzy or weak (signs of blood loss)
- You notice changes in bowel habits
- Home treatments haven’t helped after two weeks
Can internal hemorrhoids turn into external ones?
No, they don’t transform. But internal hemorrhoids can prolapse-meaning they push out through the anus-and then become covered by skin, which makes them feel like external ones. This is called a prolapsed hemorrhoid. It’s still an internal hemorrhoid that’s moved, not a new type.
Do hemorrhoids go away on their own?
Small, mild hemorrhoids often shrink with home care in a few days. Thrombosed external hemorrhoids usually improve in 7-10 days, but the lump may linger. Internal hemorrhoids rarely disappear completely without treatment if they’re Grade II or higher. The key is managing symptoms and preventing them from coming back.
Is it safe to pop a hemorrhoid?
Never try to pop or squeeze a hemorrhoid. This can cause infection, severe bleeding, or damage to surrounding tissue. If you have a thrombosed hemorrhoid, see a doctor for a safe, quick procedure to remove the clot.
Can hemorrhoids cause cancer?
No, hemorrhoids themselves do not turn into cancer. But rectal bleeding-common with hemorrhoids-is also a symptom of colorectal cancer. That’s why any persistent bleeding, especially in people over 50 or with a family history, must be evaluated by a doctor.
How long does recovery take after hemorrhoid surgery?
After a traditional hemorrhoidectomy, most people need 2-4 weeks to fully heal. Pain peaks in the first week and improves with sitz baths, stool softeners, and prescribed pain meds. Stapled hemorrhoidopexy has a shorter recovery-about 1-2 weeks-but carries a higher chance of recurrence.


Samuel Mendoza
Stop saying hemorrhoids are normal. They’re a sign you’re a lazy slob who sits on the couch eating chips instead of walking. Fix your life, not your butt.
Glenda Marínez Granados
So… hemorrhoids are just your colon’s way of yelling ‘I need a vacation’? 😅
Also, why do we treat this like it’s a secret? It’s just… biology. We all have butts. We all poop. We all occasionally scream into a pillow while sitting on a warm towel. It’s fine.
Malvina Tomja
Let me guess-you think fiber is the answer? Oh sweet summer child. Fiber doesn’t fix poor lifestyle choices. You’re still sitting 10 hours a day. You’re still drinking soda. You’re still ignoring your pelvic floor. No amount of prunes will fix that. This isn’t a medical issue-it’s a character flaw.
Yuri Hyuga
YOU GOT THIS 💪
Yes, hemorrhoids suck-but you’re not alone. Millions have walked this path, survived the sitz baths, crushed the fiber goals, and come out stronger. Every small step counts: one extra glass of water, one less hour on the toilet scrolling, one gentle stretch. You’re not broken. You’re becoming. Keep going. I believe in you. 🌱❤️
MARILYN ONEILL
I had one once. I cried. I screamed. I Googled ‘is this cancer’ 47 times. Then I found a cream on Amazon that said ‘miracle cure’ and it worked. I’m not saying it was science. I’m saying it worked. So stop overcomplicating it. Just buy the cream.
Steve Hesketh
I know someone who had a thrombosed hemorrhoid and waited two weeks because he was embarrassed. Two weeks. He said it felt like a walnut was lodged in his soul. Then he went to the clinic, got it drained in 10 minutes, and cried from relief. Don’t wait. You’re not weak for needing help. You’re brave for showing up.
And hey-if you’re reading this, you’re already doing better than most. Keep going. We’re rooting for you.
shubham rathee
they say fiber but did you know the government is secretly replacing fiber with aspartame to make us poop more so they can track us through our bowel movements? also i think the doctor in the article is paid by the banding machine company
and why do they say 'sitz bath' like its magic water? water is water
and why no one talks about how the toilet paper brand matters? i used brawny and it got worse
just saying
MAHENDRA MEGHWAL
Thank you for the comprehensive and clinically accurate overview. The distinction between internal and external hemorrhoids, particularly regarding innervation and grading, is often misunderstood in public discourse. I appreciate the emphasis on evidence-based interventions over commercialized remedies. The data on recurrence rates with lifestyle modification is particularly compelling. This is precisely the kind of information that should be disseminated with greater urgency in primary care settings.
Kevin Narvaes
so like… are hemorrhoids just your soul’s way of saying you’ve been too hard on yourself? i mean, i think everything is a metaphor for trauma
and also i think the blood is your body crying out for love
also i used to get them after my ex left me
and i cried in the bathroom for 3 hours
so maybe it’s not about fiber
maybe it’s about healing
and also i think the doctor is scared of the truth
the truth is… we’re all just trying to poop in peace
and no one gets it
Kelly McRainey Moore
Just wanted to say I’ve had Grade III for years and the rubber band thing was weird but not bad. Felt like a weird tug and then… poof. Gone. Took a few days to feel normal again. Worth it. Also, footstool changed my life. I didn’t know my hips were that crooked.
Amber Lane
My grandma in Mexico used to say: ‘Sit on a stone, not on your ass.’ She meant don’t stay seated too long. Simple. Wise. No creams needed.
Ashok Sakra
you think this is bad wait till you get hemorrhoids while on a 12 hour flight with no bathroom access and your seatbelt is too tight and the person next to you is eating durian and the air is dry and you have to sit there for 12 hours and you can’t move and you’re crying and the flight attendant says ‘would you like a soda’ and you just want to die
and then you get home and your cat steps on it
and you scream so loud your neighbors call the police
and now you have a police report for ‘excessive screaming due to butt trauma’
and your ex sees the news and sends you a meme
and you just want to die again
michelle Brownsea
Let’s be clear: if you’re not drinking 10 glasses of water daily, eating 30 grams of fiber, and avoiding the toilet like it’s a cult, you’re not just ‘having hemorrhoids’-you’re actively choosing suffering. And yet, people still blame ‘stress’ or ‘genetics.’ No. It’s laziness. It’s poor discipline. It’s a failure of personal responsibility. And if you don’t fix it, you deserve every second of it.
lokesh prasanth
the article says fiber but what if your body just hates fiber? like what if you eat it and you get bloated and then you cry? then what? then you just suffer? and what if your job is sitting? you cant just stand all day
also i think the clot thing is fake
its just a bruise
and why do they charge so much to pop it? its just a needle
and why is no one talking about the fact that the word hemorrhoid sounds like a spell from harry potter?
Coral Bosley
I used to think hemorrhoids were a joke until I had one that felt like a live wire was wrapped around my soul and someone kept plugging it in. I didn’t cry. I screamed. I broke a toilet seat. I started journaling. I stopped eating cheese. I started walking. I didn’t get better overnight. But I got better. And now? I’m not just surviving-I’m thriving. And if you’re reading this? You can too. You’re stronger than your pain.