People turn to kava for anxiety relief because it works-without the dependency risks of prescription drugs like Xanax or Valium. But here’s the catch: kava isn’t harmless, especially when mixed with other medications. If you’re taking anything for blood pressure, depression, pain, or even birth control, kava could be silently damaging your liver. And most people don’t realize it until it’s too late.
What Happens When Kava Meets Your Medications
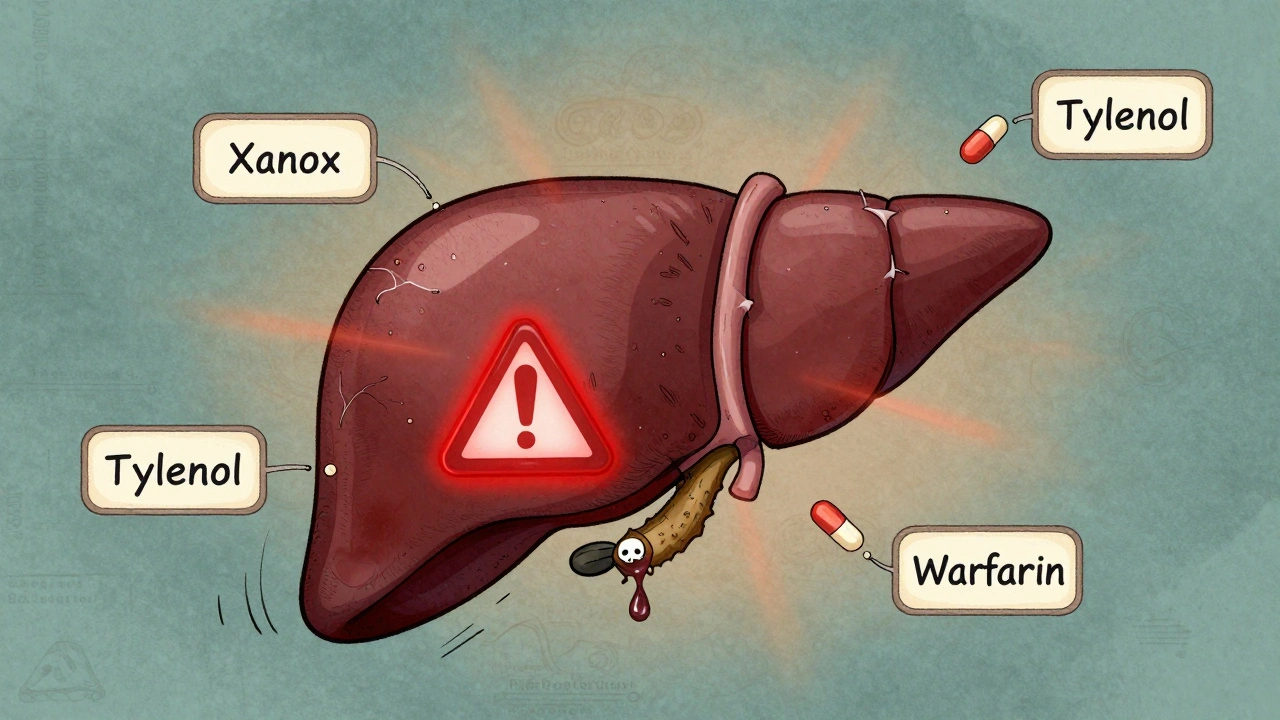
Kava doesn’t just relax your mind-it messes with your liver’s ability to process drugs. The active compounds in kava, called kavalactones, block key liver enzymes (CYP3A4, CYP2C9, CYP2C19) that break down over 80% of all prescription medications. This means drugs stay in your system longer, build up to toxic levels, or get turned into harmful byproducts. Take acetaminophen (Tylenol), for example. It’s safe at normal doses. But when combined with kava, even a regular 500 mg tablet can spike liver enzymes to dangerous levels. One documented case showed a patient’s ALT (a liver damage marker) jumping from 17 U/L to 2,442 U/L in just weeks-all while taking kava and Tylenol for migraines. That’s over 140 times the normal limit. They needed a liver transplant. The same thing happens with antidepressants like SSRIs, anti-anxiety meds, blood thinners like warfarin, and even birth control pills. Kava doesn’t just add to the load-it multiplies the risk. The FDA and WHO both warn that combining kava with other drugs is the single biggest factor behind liver failure cases.Not All Kava Is Created Equal
If you’ve heard kava is safe because Pacific Islanders have used it for thousands of years, that’s true-but only for traditional preparations. In Fiji or Vanuatu, kava is made by grinding the root and soaking it in cold water. That method pulls out the calming kavalactones while leaving behind the toxic compounds. In the U.S. and Europe, most kava supplements use ethanol or acetone to extract the active ingredients. These organic solvents pull out flavokawains-chemicals now linked directly to liver cell death. Between 2000 and 2020, nearly every case of kava-induced liver failure in Germany, Switzerland, and Canada involved these solvent-based extracts. Water-based kava tea? Almost no reports of harm. Solvent extracts? Over 50 documented liver injuries. This isn’t just about the brand-it’s about how it’s made. Check the label. If it says “ethanolic extract,” “acetonic extract,” or “standardized to 70% kavalactones,” avoid it. Look for “water-based extract” or “traditional preparation.” But even then, don’t assume it’s safe if you’re on other meds.Who’s at the Highest Risk?
Some people are just more vulnerable. The FDA lists five key risk factors:- Using solvent-extracted kava (not water-based)
- Taking high doses (over 250 mg kavalactones daily)
- Drinking alcohol regularly
- Having pre-existing liver disease (fatty liver, hepatitis, etc.)
- Having genetic variations in liver enzymes (CYP2D6 or CYP3A4 polymorphisms)

Medications That Can Turn Kava Deadly
Here’s a real list of common medications that become dangerous with kava:- Antidepressants: SSRIs (Prozac, Zoloft), SNRIs (Cymbalta), MAOIs
- Anxiolytics: Benzodiazepines (Xanax, Ativan), buspirone
- Pain relievers: Acetaminophen (Tylenol), NSAIDs (ibuprofen, naproxen)
- Blood thinners: Warfarin, apixaban, rivaroxaban
- Birth control: Pills with ethinyl estradiol or norgestimate
- Migraine meds: Rizatriptan, sumatriptan
- Cholesterol drugs: Statins (atorvastatin, simvastatin)
- Antibiotics: Erythromycin, clarithromycin
What to Do If You’re Already Taking Kava
If you’ve been using kava for months or years and are on any meds, stop immediately. Don’t wait for symptoms. Get a liver panel done-ALT, AST, bilirubin, alkaline phosphatase. Normal results don’t mean safety-they just mean damage hasn’t peaked yet. If your liver enzymes are even slightly elevated (ALT over 40 U/L), quit kava and talk to your doctor. In most cases, liver function returns to normal within weeks after stopping. But if you keep going, you could be one step away from needing a transplant. There’s no safe dose when you’re on other medications. Even 60 mg of kavalactones-a common low dose-can trigger a reaction in someone with a genetic predisposition.
Alternatives That Actually Work
You don’t need kava to manage anxiety. Safer, proven options exist:- Exercise: 30 minutes of brisk walking 5 days a week reduces anxiety as effectively as SSRIs (Journal of Clinical Psychiatry, 2021)
- Mindfulness meditation: 10 minutes daily lowers cortisol and improves sleep (Harvard Medical School, 2023)
- Valerian root: No known liver toxicity, works well for sleep and mild anxiety
- L-theanine: Found in green tea, calms without drowsiness, safe with all meds
- Cognitive behavioral therapy (CBT): Gold standard for anxiety, no side effects
What Regulators Are Saying
The European Union banned kava supplements in 2002. Canada followed in 2003. Australia restricts it to prescription-only. The FDA hasn’t banned it-but they’ve issued multiple warnings since 2002, and their 2020 Scientific Memorandum called kava “a significant hepatotoxic risk,” especially with drug interactions. The American Association for the Study of Liver Diseases (AASLD) updated their guidelines in 2022: “Patients taking medications metabolized by CYP3A4, CYP2C9, or CYP2C19 should avoid kava entirely.” That covers most common prescriptions. Meanwhile, kava sales in the U.S. grew 18% in 2021. People are still buying it. But the deaths and transplants aren’t stopping.Bottom Line: Don’t Risk It
Kava might help with anxiety. But the cost? Your liver. And once it’s damaged, you can’t reverse it. No supplement is worth a transplant. If you’re on any medication-even over-the-counter ones-skip kava. Period. If you’re already using it, get your liver checked. Talk to your doctor. Find safer alternatives. Your body doesn’t need kava. It does need a functioning liver. Protect it.Can I take kava if I don’t use any medications?
Even if you’re not on medications, kava still carries liver risks. Cases of liver damage have occurred in healthy people using high doses or solvent-extracted products. The FDA and WHO don’t recommend kava for anyone long-term, regardless of medication use. Water-based kava tea is lower risk, but not zero risk. Safer alternatives like L-theanine or meditation are better choices.
How long does it take for kava to damage the liver?
Liver damage can show up as early as 4-8 weeks with high-dose solvent extracts. In documented cases, symptoms like jaundice and nausea appeared between 12 and 17 weeks. But some people show no signs until their liver enzymes spike suddenly. There’s no safe timeline-damage can happen without warning.
Is kava tea safer than capsules or tinctures?
Yes, traditional water-based kava tea is significantly safer than capsules, tinctures, or extracts made with alcohol or acetone. Water pulls out kavalactones but leaves behind the toxic flavokawains. Most liver injury cases involve solvent-based products. But even water-based kava isn’t risk-free, especially with high doses or pre-existing liver conditions.
Can I drink alcohol while taking kava?
No. Alcohol and kava both stress the liver and inhibit the same detox enzymes. Combining them multiplies the risk of liver injury. The FDA lists heavy alcohol use as one of the top five risk factors for kava-related liver failure. Even one drink a day increases danger. Avoid alcohol completely if you’re using kava.
What should I do if I think kava damaged my liver?
Stop kava immediately. Get a liver function test (ALT, AST, bilirubin). If levels are elevated, see a hepatologist. Early detection means recovery is possible-many patients return to normal liver function after stopping kava. Delaying can lead to irreversible damage or transplant. Tell your doctor you’ve taken kava, even if you think it’s harmless.

Lauren Dare
Let me get this straight - you’re telling me that the same compound that’s been used ceremonially for centuries in the Pacific is now a ‘hepatotoxic risk’ because some asshole in Brooklyn is extracting it with acetone? The FDA warns, the EU bans, but the real villain is the supplement industry’s inability to not turn everything into a chem lab experiment. Kava tea? Fine. Solvent extracts? Criminal negligence. And yet we’re still buying it like it’s CBD gummies at a yoga retreat.
Gilbert Lacasandile
I’ve been taking kava for about 6 months for anxiety - just the water-based powder, no extracts. I’m also on a low dose of Lexapro. I didn’t realize how dangerous this could be until I read this. I’m going to stop tomorrow and get my liver checked. Thanks for laying it out so clearly. I appreciate the detail.
Lola Bchoudi
From a clinical pharmacology standpoint, the CYP450 inhibition profile of kavalactones is well-documented - particularly CYP3A4 and CYP2C9. The real issue isn’t kava itself, it’s polypharmacy in the context of unregulated nutraceuticals. Patients assume ‘natural’ = ‘safe’ and don’t disclose usage to providers. This creates dangerous pharmacokinetic synergies. We need better patient education and mandatory labeling on all kava products: ‘CONTRAINDICATED WITH CYP3A4/CYP2C9 SUBSTRATES.’
Morgan Tait
They’ve been covering this up for decades. Big Pharma hates kava because it’s cheap, natural, and doesn’t need a patent. The liver damage cases? Coincidence. The FDA warnings? A smokescreen. You think they want you to know that SSRIs cause more liver damage than kava? Nah. They’d rather you stay on pills that cost $300 a month and make you numb. Water-based kava tea is fine. It’s the corporate greed that’s poisoning people - not the root.
Darcie Streeter-Oxland
It is, without question, an alarming and well-substantiated exposition on the hepatotoxic potential of kava in the context of concomitant pharmacotherapy. One cannot help but note the conspicuous absence of any regulatory action in the United States, despite the overwhelming epidemiological evidence. The laissez-faire attitude toward herbal supplements is, frankly, indefensible.
Taya Rtichsheva
kava is fine if you dont do solvents and dont drink alcohol and dont take any meds like wtf why are people so dumb
Mona Schmidt
Thank you for this. I’ve been recommending kava to clients with anxiety, thinking water-based extracts were safe. I’ve since updated my practice guidelines. For anyone considering alternatives, L-theanine and CBT are not just safer - they’re evidence-based. The mind-body connection matters more than we’ve been led to believe. Knowledge is power, and this post is a gift.
Guylaine Lapointe
Oh please. Another ‘natural is dangerous’ fearmongering piece. My cousin in Fiji drinks kava every night since she was 15. Her liver is fine. Her stress levels? Zero. Meanwhile, Americans are on antidepressants by 18 and wonder why they feel nothing. The real crisis is our cultural obsession with pharmaceutical control. Stop blaming the plant. Blame the system that turned a sacred ritual into a $20 bottle of ‘standardized extract’.
Kathy Haverly
So let me get this straight - you’re telling me that after 20 years of research, the only reason kava is dangerous is because people are stupid enough to combine it with everything? That’s not a risk. That’s a failure of education. And yet you still sell it. You still market it. You still let people believe it’s ‘safe’ if they ‘do it right.’ The system is rigged. This isn’t about liver enzymes - it’s about profit. And you’re complicit.
Andrea DeWinter
i took kava for a month with my blood pressure med and felt fine so maybe its not that bad idk just saying
Steve Sullivan
Bro… the liver is like your body’s Uber driver for toxins. Kava? It’s the guy who hijacks the car, deletes the GPS, and says ‘trust me, I know a shortcut.’ Then you wake up in a ditch with your meds still in your system and no idea how you got there. 🚗💨🩸 Maybe try meditation? Or a walk? Your liver will thank you. And yes, I’m an emoji guy. Deal with it.
George Taylor
...And yet, the fact remains - there are documented cases of liver failure. Not hypothetical. Not ‘maybe.’ Not ‘some people.’ Actual, measurable, clinical, life-threatening events. And you’re casually dismissing it because ‘my cousin in Fiji’? That’s not data. That’s anecdote. And anecdote doesn’t save lives. Evidence does.
Chris Marel
This is powerful. I’m from Nigeria, and we don’t have kava here - but I’ve seen how people treat herbal remedies like they’re immune to side effects. Your post reminds me of how we need to talk about traditional medicine with the same rigor we give pharmaceuticals. Not to dismiss culture, but to protect it. Thank you for the clarity.