What Is Hyperkalemia in Chronic Kidney Disease?
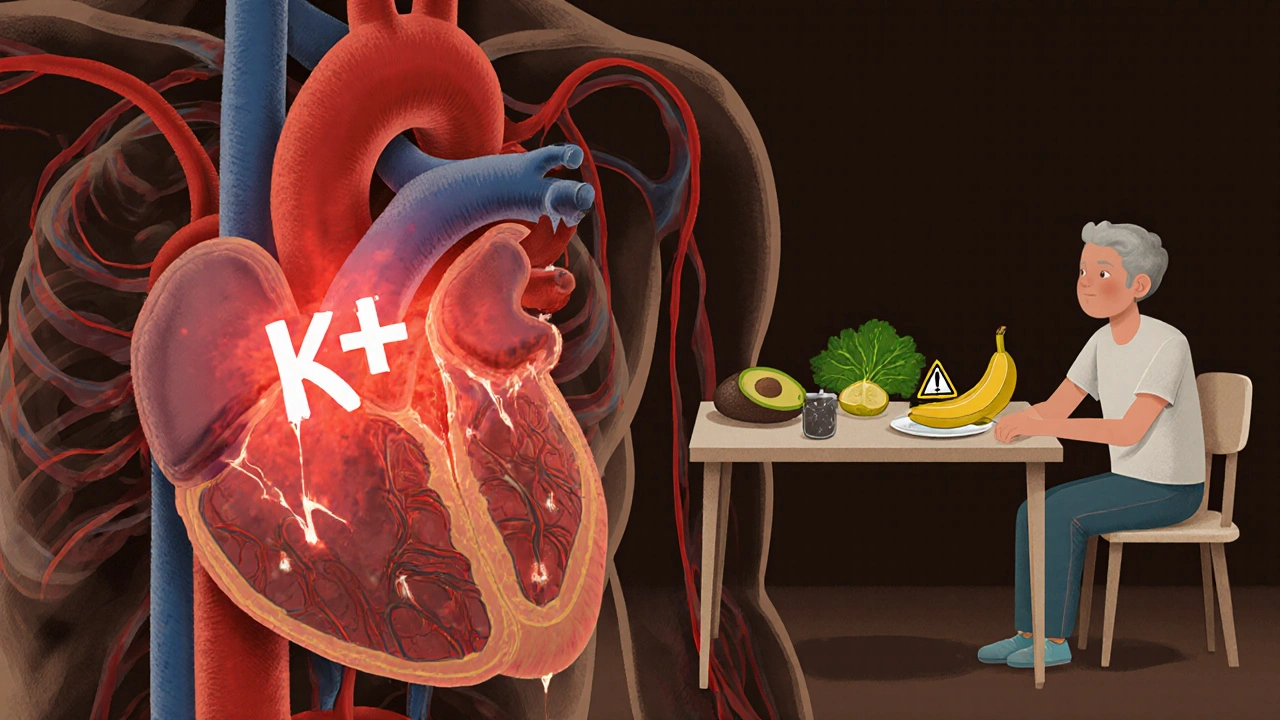
When your kidneys can't filter blood properly, potassium builds up in your bloodstream. That’s hyperkalemia - a dangerous spike in blood potassium levels, usually above 5.0 mmol/L. In people with chronic kidney disease (CKD), this isn’t rare. About 40-50% of those with advanced CKD (stages 3b-5) will experience it at some point. It’s not just a lab number. High potassium can stop your heart.
Most people don’t feel symptoms until it’s serious. Then comes muscle weakness, irregular heartbeat, or sudden chest pain. The real danger? Many patients are on medications like ACE inhibitors or ARBs - drugs that protect the heart and kidneys but also raise potassium. So doctors face a tough choice: keep the heart-protecting drugs, or lower them and risk faster kidney or heart damage.
Why Potassium Becomes a Problem in CKD
Your kidneys normally remove extra potassium through urine. But when kidney function drops below 30 mL/min (stage 4 CKD), that system breaks down. Even small increases in dietary potassium can push levels into the danger zone. The problem gets worse if you’re also taking diuretics that stop working in late-stage CKD, or if you have diabetes or heart failure - both common in CKD patients.
And here’s the catch: the older you get, the more likely you are to be on multiple medications. The average CKD patient takes 7.2 different drugs daily. Some of these - like NSAIDs, beta-blockers, or spironolactone - also interfere with potassium balance. It’s not one thing. It’s a perfect storm.
Dietary Limits: How Much Potassium Is Safe?
There’s no one-size-fits-all diet. For early-stage CKD (stages 1-3a), you don’t need to cut potassium drastically. The goal is to avoid excessive intake - no giant bowls of spinach, no 5 bananas a day. But if you’re in stage 3b or worse, you need to be strict: aim for 2,000-3,000 mg per day (51-77 mmol).
Here’s what that means in real food:
- One medium banana = 422 mg
- One baked potato = 926 mg
- One cup of orange juice = 496 mg
- Half a cup of cooked spinach = 420 mg
- One avocado = 708 mg
That’s just four foods - you’re already over 2,000 mg before lunch. So you need tricks. Boiling potatoes, carrots, or beets reduces potassium by 50%. Skip the broth in soups - it’s packed with potassium. Choose apples, berries, cabbage, and green beans instead. A renal dietitian can help you build a meal plan that doesn’t leave you hungry or isolated.
But here’s the hard truth: only 37% of patients stick to these limits long-term. Social events, lack of time, or simple confusion make it tough. That’s why newer tools - like apps that scan food barcodes and calculate potassium content - are helping. One pilot study showed a 32% improvement in adherence just by using these tools.

Emergency Treatment: What Happens When Potassium Hits 6.0?
If your potassium hits 6.0 mmol/L or higher - especially with ECG changes like widened QRS or peaked T-waves - this is a medical emergency. You need treatment right now, not tomorrow.
Doctors follow a clear sequence:
- Calcium gluconate (10 mL IV over 2-5 minutes): This doesn’t lower potassium, but it protects your heart muscle from the electrical chaos. It works in 1-3 minutes and lasts about an hour.
- Insulin and glucose (10 units insulin + 50 mL of 50% dextrose): This pulls potassium into your cells. It lowers levels by 0.5-1.5 mmol/L within 30 minutes. But watch out - 10-15% of patients get dangerously low blood sugar. You’ll need glucose monitoring for hours after.
- Sodium bicarbonate (50-100 mmol IV): Only if you’re also acidotic (bicarbonate below 22 mmol/L). It works fast - 5-10 minutes - but it’s not always needed.
These steps buy time. But they don’t fix the root problem. You still need to remove the extra potassium from your body. That’s where binders come in.
Chronic Management: The New Generation of Potassium Binders
For long-term control, older drugs like sodium polystyrene sulfonate (SPS) are fading out. They’re messy - you mix them with water or sorbitol, they taste awful, and they carry a 0.5-1% risk of deadly bowel damage.
Two new binders changed everything:
- Sodium zirconium cyclosilicate (SZC, brand Lokelma): Works in under an hour. Lowers potassium by 1.0-1.4 mmol/L fast. But it adds sodium - about 1.2 grams a day. That’s a problem if you have heart failure or swelling.
- Patiromer (brand Veltassa): Slower - takes 4-8 hours to work. But it’s sodium-free. Better for heart patients. Side effects? Constipation (14.2%) and low magnesium (18.7%).
Studies show these drugs let people stay on life-saving heart medications. In one trial, 78% of patients on patiromer kept their full RAASi dose. Without it, only 38% could. That’s huge.
Cost is a barrier. SPS costs about £47 a month. Patiromer? £286. SZC? Even more. Many clinics can’t afford them. But the cost of a hyperkalemia hospital visit? Around $12,450 in the U.S. That’s why more hospitals are pushing for earlier use - even if it’s expensive upfront.
Monitoring and Follow-Up: Staying Safe Long-Term
Checking potassium isn’t optional. If you start or increase a RAASi drug, get your levels tested within 1-2 weeks. Then every 3-6 months if you’re stable. But if you feel weak, dizzy, or your heart skips - get tested immediately.
Many clinics now use electronic alerts. When your potassium hits 5.0 mmol/L, the system flags it. A pharmacist calls. A dietitian schedules a visit. It’s not magic - it’s structure. One UK clinic boosted RAASi continuation from 52% to 81% just by adding routine monitoring.
And don’t forget medication timing. Patiromer can block absorption of thyroid meds, antibiotics, or blood pressure drugs if taken too close together. You need to space them at least 3 hours apart. A pharmacist should review your whole list every 6 months.
What’s Next? The Future of Hyperkalemia Care
Experts are moving toward precision management. Instead of a blanket 2,000 mg limit, they’re testing urine potassium tests to tailor diets to your body’s actual output. New drugs like tenapanor - which blocks potassium absorption in the gut - are in trials. One early study showed a 0.48 mmol/L drop in just weeks.
By 2027, experts predict 75% of CKD patients on heart-protecting drugs will also be on a potassium binder. That’s a massive shift. It means fewer emergency rooms, fewer deaths, and better quality of life.
But the biggest win? You don’t have to choose between protecting your heart and keeping potassium low anymore. With the right tools, you can do both.
Key Takeaways
- Hyperkalemia in CKD is common and deadly - levels above 5.0 mmol/L need attention.
- Emergency treatment requires calcium, insulin-glucose, and sometimes bicarbonate - fast action saves lives.
- For chronic control, newer binders (SZC and patiromer) are safer and more effective than old ones like SPS.
- Dietary potassium limits are 2,000-3,000 mg/day in advanced CKD. Boiling vegetables helps reduce content.
- Monitoring every 3-6 months and careful medication timing are critical to avoid complications.

Shivam Goel
This is solid. But let’s be real-most patients don’t even know what 'mmol/L' means. You throw around numbers like they’re grocery lists, but the guy on dialysis in rural India? He’s just trying to eat something that doesn’t make him feel like he’s being electrocuted. You need visuals. Infographics. Maybe even voice notes in Hindi or Tamil. This article reads like a textbook written by someone who’s never held a banana in their hand.
Amy Hutchinson
I’m a nurse in Arizona and I’ve seen this play out 37 times. One guy ate a whole bag of salt substitute because he thought it was ‘healthy.’ It wasn’t. He coded. We saved him. But his wife cried for an hour because she thought potassium was just ‘that thing in bananas.’ This isn’t medicine-it’s a cultural literacy crisis.
Archana Jha
Wait… so you’re telling me the pharmaceutical companies WROTE this article?!! They *want* you to be on binders because they make $300/month off you. SPS is dangerous? Nah. They just don’t want you to use the $47 drug because it’s not profitable. And those apps? They’re tracking your food intake to sell to insurers. You think they care about your heart? They care about your insurance premiums. The government’s in on it too. They don’t want you healthy-they want you *managed*. #BigPharmaLies
Aki Jones
The structural inequities embedded in renal care are unconscionable. The pharmacoeconomic calculus prioritizes cost containment over physiological integrity, resulting in iatrogenic harm via suboptimal binder utilization. Furthermore, the commodification of dietary adherence through algorithmic surveillance tools represents a neo-liberal encroachment upon bodily autonomy. The 32% adherence increase? A statistical mirage-masked by selection bias and unmeasured confounders. This is not progress. It’s performative medicine.
Jefriady Dahri
I’m a kidney patient myself. Been on dialysis for 6 years. This article? It’s the first one that didn’t make me feel like a problem to be fixed. 💙 Boiling veggies? I’ve been doing it for years. My mom taught me. And yeah, the binders are pricey-but I’d rather pay $286 than end up in the ER screaming because my heart forgot how to beat. Keep sharing this stuff. You’re helping people like me feel seen. 🙏
Andrew McAfee
In India we just eat rice and lentils and pray to Shiva and it works fine. Why make it so complicated. Potassium is just a number. People in America think everything is a crisis. My uncle had CKD for 20 years and never took a binder. He lived to 82. Maybe the real problem is overmedicating
Elise Lakey
I really appreciate how you broke down the emergency protocol. I’ve been reading about this for months but never understood why calcium gluconate comes first. It makes sense now-it’s not about fixing the potassium, it’s about buying time. Thank you. I’m sharing this with my dad’s nephrologist.
Roscoe Howard
The notion that a developing nation can adequately manage hyperkalemia without the infrastructure of a first-world healthcare system is not only naïve-it is irresponsible. The United States leads the world in renal outcomes precisely because we invest in precision therapeutics. To suggest that boiling vegetables is a viable alternative to patented, FDA-approved binders is not just medically unsound-it is an affront to the principles of evidence-based medicine. This is not a debate. It is a failure of intellectual rigor.
Kimberley Chronicle
I’m a renal dietitian in London, and I’ve started using the barcode scanner apps with my patients. It’s been transformative. One woman, 78, used to skip meals because she was terrified of potassium. Now she eats berries and green beans and says she feels like she’s ‘eating again.’ The binders? Expensive, yes. But when you factor in ER visits and ICU stays? It’s a bargain. We’re starting a pilot to cover them under NHS chronic care bundles. Small steps, but they matter.