Diuretic Selection Tool
Choose Your Clinical Scenario
Recommended Diuretic
Choose a scenario to see recommendation...
When doctors need to get rid of excess fluid quickly, they often reach for Lasix. But is it always the best choice? This guide breaks down how Lasix (Furosemide) stacks up against the most common alternatives, so you can understand which drug fits each clinical picture.
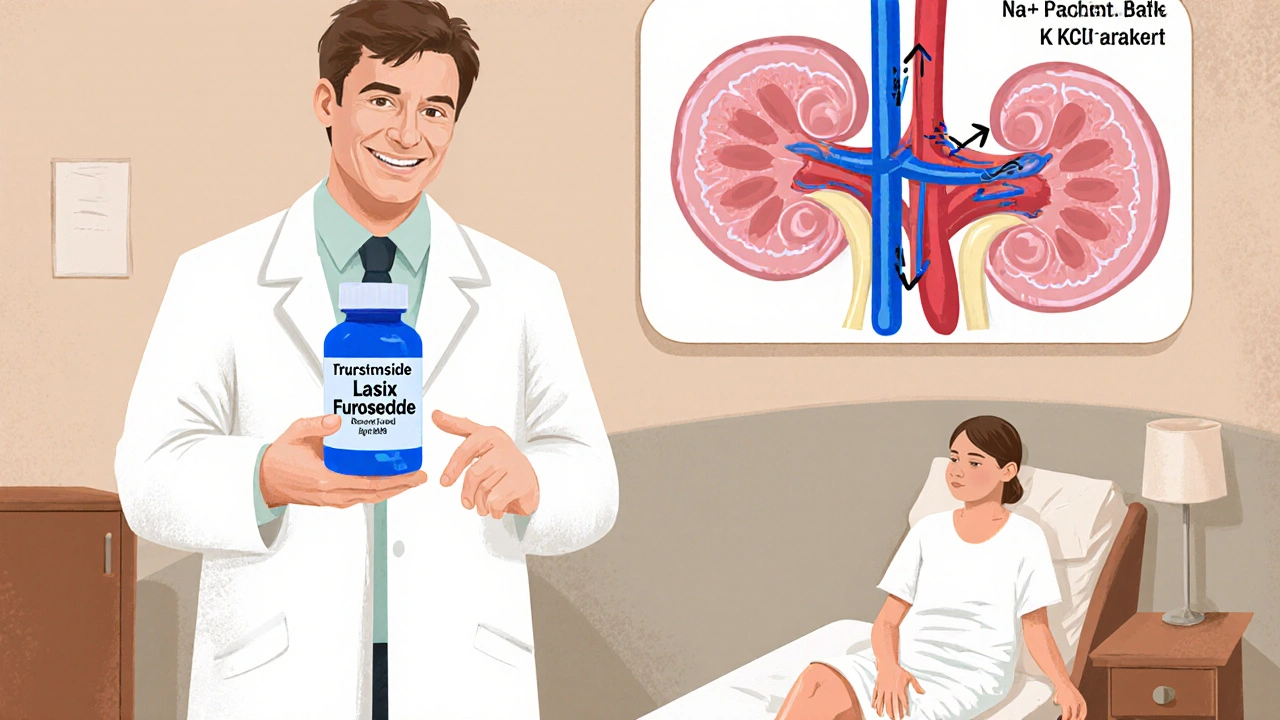
What is Lasix (Furosemide)?
Lasix (Furosemide) is a potent loop diuretic that blocks sodium‑chloride reabsorption in the thick ascending limb of the nephron. Known as frusemide outside the United States, it was first marketed in the 1960s and quickly became the go‑to medication for conditions like pulmonary edema, heart failure, and severe hypertension.
How Lasix Works: The Pharmacology in Plain English
Lasix targets the Na⁺‑K⁺‑2Cl⁻ cotransporter (NKCC2) in the renal loop of Henle. By inhibiting this transporter, it forces the kidneys to excrete large volumes of sodium, chloride, and water. The result is a rapid drop in intravascular volume, which eases fluid overload and lowers blood pressure within hours.
Key Factors When Comparing Diuretics
- Potency: How much fluid loss does a standard dose produce?
- Onset and Duration: How quickly does the drug act, and how long does its effect last?
- Indications: Which diseases or symptoms is it approved for?
- Side‑Effect Profile: Risks such as electrolyte imbalance, ototoxicity, or kidney injury.
- Renal Clearance: How the drug is eliminated, which matters in patients with reduced kidney function.
- Cost & Availability: Generic vs brand, insurance coverage, and regional formularies.
Alternative Loop Diuretics
Loop diuretics share the same site of action as Lasix but differ in potency, half‑life, and tolerability.
Bumetanide is a loop diuretic about 40 % more potent than Lasix, with a shorter half‑life of 1‑2 hours. It’s often chosen when a rapid, controllable diuresis is needed, such as in acute decompensated heart failure.
Torsemide offers a longer duration (up to 12 hours) and a more predictable dose‑response curve. Its bioavailability is higher (≈80 %) than Lasix, making it useful for outpatient chronic management.
Ethacrynic acid is the only non‑sulfonamide loop diuretic, which matters for patients allergic to sulfa drugs. It’s less potent than Lasix and carries a higher risk of ototoxicity, so it’s usually a second‑line option.

Thiazide Diuretics: A Different Class
Thiazides act farther downstream in the distal convoluted tubule. They’re weaker than loop diuretics but excellent for long‑term blood‑pressure control.
Hydrochlorothiazide is the most widely prescribed thiazide. It reduces calcium excretion, which can be beneficial for patients with osteoporosis, but it may raise uric acid levels.
Chlorthalidone, not covered in depth here, is another thiazide‑like drug with a longer half‑life, often preferred for hypertension.
Potassium‑Sparing Diuretics
These agents limit potassium loss, making them useful in combination therapy.
Spironolactone antagonizes aldosterone in the collecting duct, helping treat resistant hypertension and heart‑failure‑related edema while conserving potassium.
Amiloride is another potassium‑sparing option, typically added to a loop or thiazide when hypokalemia becomes a problem.
Side‑Effect Profiles: What to Watch For
All diuretics can cause electrolyte disturbances, but the pattern varies:
- Loop diuretics (Lasix, Bumetanide, Torsemide, Ethacrynic acid) → low potassium, low magnesium, possible ototoxicity, hyperuricemia.
- Thiazides → low potassium, low sodium, hypercalcemia, hyperglycemia, hyperuricemia.
- Potassium‑sparing → hyperkalemia, especially when combined with ACE inhibitors.
Comparative Table: Lasix vs Common Alternatives
| Drug | Potency (relative to Lasix) | Half‑Life | Typical Indications | Main Side‑Effects | Cost (US$ per 20 mg) |
|---|---|---|---|---|---|
| Lasix (Furosemide) | 1× (baseline) | 1.5-2 hours | Acute pulmonary edema, heart failure, renal failure, severe hypertension | Hypokalemia, ototoxicity (high dose), dehydration | ~0.10 |
| Bumetanide | 1.5-2× | 1-2 hours | Same as Lasix, but useful when rapid diuresis needed | Similar electrolyte loss, less ototoxicity at equi‑dose | ~0.25 |
| Torsemide | 0.8-1× | 3-6 hours | Chronic heart failure, hypertension, edema | Lower risk of hypokalemia, mild metabolic alkalosis | ~0.30 |
| Ethacrynic acid | ≈1× | 1-2 hours | Sulfa‑allergic patients needing loop diuresis | Higher ototoxicity, potential for severe leukopenia | ~0.45 |
| Hydrochlorothiazide | 0.05× (much weaker) | 6-15 hours | Hypertension, mild edema, calcium‑sparing | Hypokalemia, hypercalcemia, hyperglycemia | ~0.08 |
| Spironolactone | 0.02× (weak natriuresis) | 1.4-2.5 hours (active metabolites 10-30 hours) | Resistant hypertension, heart‑failure with reduced EF, hyperaldosteronism | Hyperkalemia, gynecomastia (male patients) | ~0.12 |
Choosing the Right Diuretic: Practical Scenarios
Scenario 1 - Rapid decongestion in acute heart failure: Lasix or Bumetanide are preferred because they move large volumes quickly. Bumetanide may be favored if the patient needs a slightly stronger effect per milligram.
Scenario 2 - Chronic outpatient management of hypertension with mild edema: A thiazide like Hydrochlorothiazide provides steady blood‑pressure control with less frequent dosing.
Scenario 3 - Sulfa allergy: Ethacrynic acid becomes the only loop diuretic option, though clinicians monitor hearing closely.
Scenario 4 - Preventing potassium loss while on a loop diuretic: Adding Spironolactone or low‑dose Amiloride can balance electrolytes without causing severe hyperkalaemia.
Pitfalls to Avoid
- Don’t assume all loop diuretics are interchangeable; dosing ratios differ.
- Watch renal function closely - a sudden rise in creatinine may mean the diuretic is too aggressive.
- Always replace lost potassium, especially with Lasix, Bumetanide, or Torsemide.
- Be cautious with concurrent ototoxic drugs (e.g., aminoglycosides) while on high‑dose loop diuretics.
Bottom Line
Lasix remains the workhorse for fast, strong diuresis, but alternatives like Bumetanide, Torsemide, and thiazides each have niches where they outperform it. Understanding potency, half‑life, side‑effects, and patient‑specific factors lets clinicians tailor therapy rather than defaulting to a one‑size‑fits‑all approach.
Can I switch from Lasix to a thiazide diuretic for long‑term blood pressure control?
Yes, many patients start on Lasix for acute fluid overload and later transition to a thiazide like Hydrochlorothiazide for chronic hypertension. The switch reduces the risk of severe electrolyte loss while still providing modest diuresis.
Is Bumetanide more dangerous than Lasix?
Bumetanide is more potent per milligram, so dosing errors can happen if you simply replace Lasix milligram‑for‑milligram. When used correctly, its safety profile is similar, but the higher potency means careful monitoring of electrolytes.
Why might a doctor prescribe Ethacrynic acid instead of Lasix?
Ethacrynic acid is the only non‑sulfonamide loop diuretic, so it’s used for patients with a documented sulfa allergy. It’s less common because it carries a higher ototoxicity risk.
Can I take Spironolactone together with Lasix?
Combining a loop diuretic with a potassium‑sparing agent like Spironolactone is a common strategy to prevent hypokalemia. However, regular potassium checks are essential to avoid hyperkalaemia.
What lab values should I monitor while on Lasix?
Key labs include serum potassium, magnesium, creatinine, and blood urea nitrogen. If the dose exceeds 80 mg IV, also monitor hearing if the patient reports tinnitus.

Tamara Schäfer
When you think about the way our bodies handle excess fluid, it's almost poetic how a single molecule can tip the balance between comfort and crisis.
Lasix, with its potent loop action, serves as the quick‑draw sheriff in the renal neighborhood, flushing out sodium and water in a matter of hours.
This rapid decongestion can be a lifeline for someone drowning in pulmonary edema, yet the same power can also strip away vital electrolytes if we aren't careful.
One must remember that potency is a double‑edged sword: the more fluid you pull, the greater the risk of hypokalemia, ototoxicity, and even a sudden rise in creatinine.
Alternative loops like Bumetanide give you a hotter punch per milligram, while Torsemide stretches its effect over a longer day, which can be a blessing for outpatient management.
For patients allergic to sulfa, Ethacrynic acid steps in as the lone non‑sulfonamide, but its higher ototoxic potential reminds us that no drug is without trade‑offs.
Thiazides on the other hand, such as Hydrochlorothiazide, work farther down the nephron and are gentler, making them suitable for chronic blood pressure control rather than an emergency dump.
When you pair a loop with a potassium‑sparing agent like Spironolactone, you balance the scales, reducing the chance of dangerous hypokalemia.
This approach definatly helps avoid the dreaded low potassium trap.
However, this combo demands vigilant potassium monitoring, especially if the patient is also on ACE inhibitors.
Cost considerations also play a role; while generic Lasix can be pennies per dose, newer agents like Torsemide may carry a higher price tag that insurance plans balk at.
The renal clearance of each drug dictates dosing adjustments in chronic kidney disease, with reduced clearance necessitating lower or less frequent doses.
Clinical scenarios guide the choice: acute flash decongestion favors Lasix or Bumetanide, chronic outpatient edema leans toward Torsemide, and sulfa allergy forces Ethacrynic acid into the spotlight.
In the grand scheme, the art of diuretic selection lies in matching potency, half‑life, side‑effect profile, and patient specifics rather than blindly reaching for the most famous name.
So, while Lasix remains the workhorse, the toolbox is richer than you might think, and a thoughtful clinician can tailor therapy to each individual's needs.
Remember, the goal is not just to make the urine flow, but to keep the patient safe, stable, and hopeful about their reccover.
Tamara Tioran-Harrison
It is, of course, entirely astonishing that anyone would consider deviating from the time‑tested, universally acclaimed supremacy of Lasix when faced with the monumental task of fluid removal, a notion that simply defies the very principles of modern medicine 😊.
kevin burton
For clinicians who prefer a straightforward approach, remember that Lasix’s half‑life is roughly 1.5‑2 hours, so dosing every 6‑8 hours usually maintains adequate diuresis without excessive peaks.
In patients with reduced kidney function, start with a lower dose and titrate based on urine output and serum electrolytes.
Monitoring potassium, magnesium, and creatinine at baseline and after any dose change is essential to avoid complications.
Whenever possible, combine a loop diuretic with a potassium‑sparing agent to mitigate hypokalemia, especially if the patient is also on an ACE inhibitor.
Max Lilleyman
While the hyper‑formal adulation of Lasix might sound impressive, the reality is that such blind reverence often ignores patient‑specific nuances, leading to over‑diuresis and preventable electrolyte disasters. 😒🔍
Buddy Bryan
Listen, the "straightforward approach" you tout is fine for textbook cases, but real‑world patients throw curveballs like concurrent NSAID use, variable dietary sodium, and hidden sulfa allergies that demand a more aggressive, individualized plan. Adjust the loop dose upward if the edema persists, but never forget to re‑check labs within 24 hours of any change-no excuses.
Jonah O
What most people fail to notice is that the pharmaceutical giants have secretly engineered the so‑called "alternatives" to keep doctors dependent on a rotating menu of patents, ensuring a constant stream of profit while the true solution-balanced fluid homeostasis-remains suppressed.
Take for example the subtle tweak in Bumetanide's formulation that allegedly "improves bioavailability" but actually masks a hidden ototoxic additive, a detail that never makes it into the glossy pamphlets.
Even the naming conventions are a smokescreen: "Torsemide" sounds exotic, yet its metabolic pathway is practically identical to Lasix, a fact that regulators conveniently overlook.
Ask yourself why Ethacrynic acid, the only non‑sulfonamide, is priced higher than its sulfa cousins despite its higher risk profile-it's a classic case of engineered scarcity.
In short, the diuretic market is a carefully curated illusion, and only the most vigilant clinicians can see through the layers of obfuscation.
Aaron Kuan
Vivid colors swirl, kidneys dance, truth hides.
Brett Witcher
One must acknowledge that the discourse surrounding loop diuretics often suffers from a lamentable paucity of rigorous pharmacodynamic nuance, wherein the casual reader is presented with an oversimplified tableau of potency versus half‑life. A meticulous examination reveals that the structural heterogeneity of the chloro‑substituted phenoxy moiety in Torsemide confers its superior bioavailability, whereas the mercurial ester linkage in Bumetanide accounts for its rapid onset. Moreover, the colloquial conflation of "stronger" with "more dangerous" neglects the pivotal role of dosing intervals and renal clearance in shaping the therapeutic window. Hence, any substantive recommendation must be predicated upon a stratified analysis of patient comorbidities, electrolyte trends, and economic considerations, rather than an indiscriminate reliance upon brand recognition.