Triptan Safety Checker
Check Your Medication Safety
Enter medications you're currently taking to assess risks with triptans.
Triptans are the go-to treatment for many people with moderate to severe migraines. They work fast, often bringing relief in under two hours. But for every person who finds relief, another hits a wall-side effects, no improvement, or worse, dangerous interactions. If you’ve ever taken a triptan and felt chest tightness, dizziness, or had your migraine come back worse after a few hours, you’re not alone. And if you’re on an SSRI or SNRI, you might be at risk without even knowing it.
What Triptans Actually Do
Triptans aren’t just painkillers. They’re targeted drugs that lock onto serotonin receptors in your brain and blood vessels. Specifically, they activate 5-HT1B and 5-HT1D receptors. This causes two things: the swollen blood vessels around your brain shrink back down, and the nerves that fire off pain signals stop releasing chemicals like CGRP and substance P. That’s why they work so well for migraines-they’re fixing the actual problem, not just masking the pain.
There are seven FDA-approved triptans: sumatriptan, rizatriptan, zolmitriptan, naratriptan, frovatriptan, eletriptan, and almotriptan. They all end in “-triptan,” which makes them easy to spot on a prescription. But they’re not the same. Sumatriptan works fast but wears off quickly. Frovatriptan lasts almost a full day. Rizatriptan hits harder in the first two hours. Eletriptan has the highest success rate for complete pain relief at two hours-75% in some studies. But if you take it too late, none of them work as well.
When Triptans Don’t Work
One in three people with migraines don’t get good relief from any triptan. And about one in five never respond to any of them, no matter how many they try. Why? It’s not just bad luck. Your genetics, how your body processes serotonin, and even the timing of your attack play a role.
Triptans work best when taken at the first sign of pain-not during the aura, not when you’re just feeling “off.” If you wait too long, the blood vessels are already fully dilated, and the nerves are firing nonstop. Studies show taking a triptan within 20 minutes of headache onset gives you the best shot at stopping it. If you wait an hour or more, effectiveness drops by 30% or more.
Another big reason triptans fail? Cutaneous allodynia. That’s when your skin becomes painfully sensitive-brushing your hair, wearing glasses, or even a light touch on your scalp hurts. If you have this, triptans are only about 30-40% effective. Without it, they work 70-80% of the time. That’s why some people swear by one triptan and hate another-it’s not the drug, it’s the stage of their migraine.
Big Red Flags: Contraindications
Triptans are safe for most people. But they’re absolutely not for everyone. If you have heart disease, a past heart attack, uncontrolled high blood pressure, or a history of stroke or transient ischemic attack (TIA), you should never take a triptan. These drugs constrict blood vessels-and if your arteries are already narrowed, that can trigger a heart attack or stroke.
Even if you don’t have a diagnosis, if you’re over 40 and have risk factors like smoking, diabetes, or high cholesterol, your doctor should screen you before prescribing a triptan. There’s a documented risk: one heart attack per 10,000 patient-years of sumatriptan use. That’s rare, but not zero. And it’s avoidable.
Severe liver disease is another no-go. Triptans are broken down in the liver. If your liver can’t handle it, the drug builds up and increases side effects. Same goes for people with peripheral vascular disease-poor circulation in the legs or arms. Triptans can make that worse.
Drug Interactions You Can’t Ignore
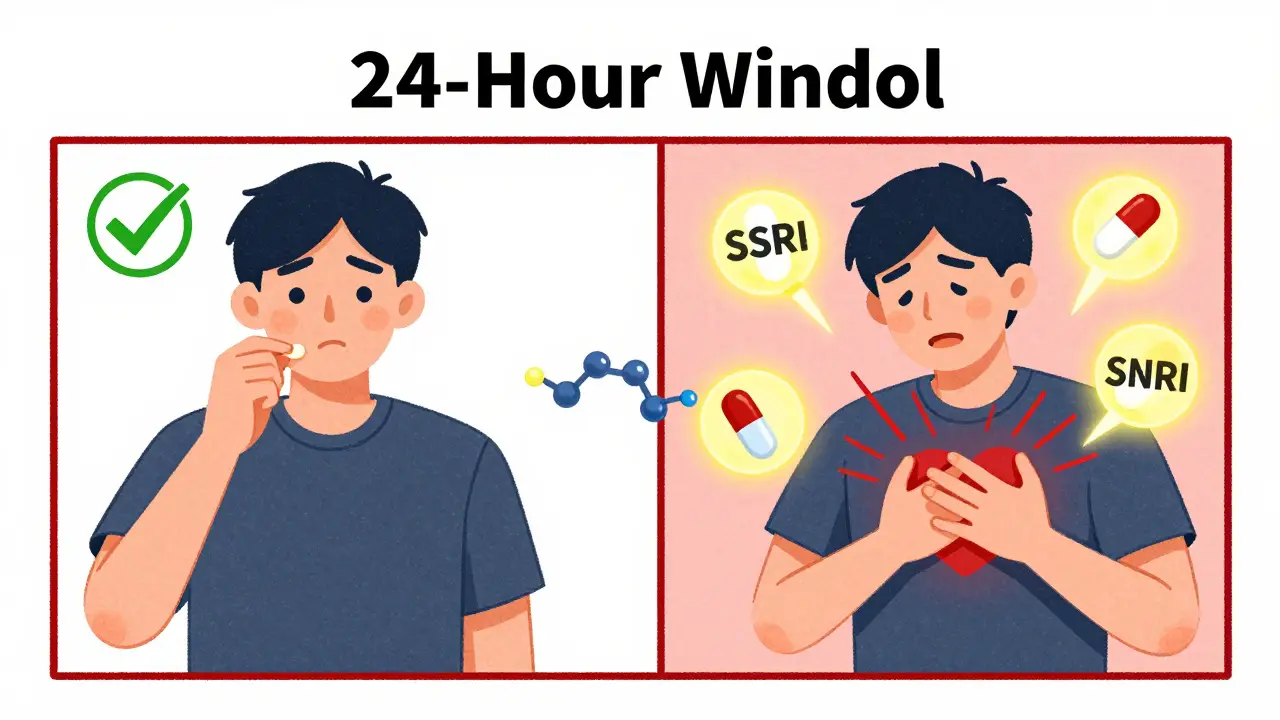
The biggest interaction risk is with antidepressants-SSRIs like sertraline or SNRIs like venlafaxine. Both raise serotonin levels. Triptans also activate serotonin receptors. Put them together, and you risk serotonin syndrome: a rare but dangerous condition where your body has too much serotonin. Symptoms include confusion, rapid heart rate, high blood pressure, muscle rigidity, fever, and seizures.
It’s rare-only a handful of confirmed cases in the medical literature-but it’s real. And it’s preventable. If you’re on an SSRI or SNRI, tell your doctor before taking a triptan. Don’t assume it’s fine because you’ve taken both before. Your risk goes up with higher doses or if you start a new antidepressant.
Another interaction to watch for is with ergotamines (like Cafergot) or other migraine drugs like lasmiditan. Never take a triptan within 24 hours of an ergotamine. They both constrict blood vessels, and stacking them can cause dangerous spasms.
Side Effects: More Common Than You Think
Most people tolerate triptans well. But side effects are normal-and often underreported.
- 5-7% feel chest, throat, or jaw tightness. It’s not a heart attack-it’s the drug tightening blood vessels. But if you’ve never had this before, get it checked.
- 4-10% get dizzy or lightheaded.
- 3-8% feel unusually tired or sleepy.
- Some report nausea, flushing, or a metallic taste.
These usually fade within an hour. But if you’ve had chest tightness before, you might avoid triptans altogether. That’s okay. There are alternatives.

Overuse and the Risk of Worsening Migraines
Triptans are powerful. But using them too often turns them into the problem.
Using a triptan more than 10 days a month can trigger medication-overuse headache (MOH). That’s when your headaches become daily, worse, and harder to treat. The International Headache Society says: no more than two doses per day, and never more than 10 days a month. That’s it.
And here’s the catch: if you’re taking triptans for mild migraines or using them preventively, you’re already on the path to MOH. Triptans are for acute attacks-only when the pain is clearly there. Don’t take them “just in case.”
What If Triptans Don’t Work for You?
Don’t give up. About 30-40% of people who don’t respond to one triptan respond to another. It’s not about trying them all-it’s about matching the drug to your migraine pattern.
If you get long-lasting migraines, frovatriptan’s 26-hour half-life might be better. If you need fast relief, rizatriptan or zolmitriptan nasal spray work quicker than pills. If nausea is a problem, the orally disintegrating tablets (like rizatriptan ODT) are easier to take.
And if triptans still don’t help? Newer options exist. Gepants (like ubrogepant and rimegepant) block CGRP without constricting blood vessels. They’re safe for people with heart disease. Ditans (like lasmiditan) target a different serotonin receptor-no vasoconstriction at all. These aren’t first-line yet, but they’re game-changers for those who can’t use triptans.
The Bigger Picture: Triptans in 2025
Triptans have been the backbone of migraine treatment for over 30 years. Over 300 million prescriptions have been written since sumatriptan hit the market in 1991. They’re cheap, effective, and well-studied.
But the landscape is changing. New drugs are safer for people with heart risks. Insurance is starting to cover them more widely. By 2027, triptans may drop from 45% to 38% of the acute migraine market.
Still, for most people without heart issues, triptans remain the fastest, most reliable option. The key isn’t to avoid them-it’s to use them right. Know your limits. Know your risks. Know when to switch. And never take them without understanding the warning signs.
Can I take a triptan with ibuprofen or naproxen?
Yes, combining a triptan with an NSAID like naproxen or ibuprofen is not only safe-it’s often more effective. Studies show that sumatriptan 85 mg plus naproxen sodium 500 mg gives you a 27% chance of being pain-free at two hours, compared to 18% with sumatriptan alone. This combo is recommended for people who don’t get full relief from triptans alone. Just make sure you’re not exceeding daily limits for the NSAID, especially if you have stomach or kidney issues.
Why do I feel tightness in my chest after taking a triptan?
That tightness is a common side effect caused by the drug narrowing blood vessels-not just in your brain, but in your chest too. It’s not a heart attack, but it can feel like one. It usually lasts less than 30 minutes. If you’ve never had this before, or if it lasts longer than an hour, get checked. If you have heart disease, this reaction is a red flag-you should avoid triptans entirely.
Can I take two different triptans in one day?
No. Never take two different triptans in the same 24-hour period. Even if one didn’t work, switching to another doesn’t improve outcomes-it just increases your risk of side effects and medication-overuse headache. If one triptan fails, wait until the next attack to try a different one. Your doctor can help you choose which one to switch to based on your migraine pattern.
Are triptans safe during pregnancy?
There’s not enough data to say triptans are completely safe during pregnancy. Most doctors avoid them in the first trimester unless absolutely necessary. If you’re pregnant and have severe migraines, your doctor may recommend acetaminophen, rest, or non-pharmacological options first. If a triptan is needed, sumatriptan has the most safety data and is often the first choice-but only after weighing risks and benefits.
What should I do if my migraine comes back after a triptan?
Rebound migraines within 24 hours happen in 15-40% of users, depending on the triptan. If this happens, don’t take another dose right away. Wait at least 24 hours before trying a different triptan or another treatment. If this happens often, you might need a preventive medication, not just more acute ones. Talk to your doctor about options like beta-blockers, CGRP inhibitors, or lifestyle changes to reduce attack frequency.

Aayush Khandelwal
Triptans are basically the serotonin ballet of neurology-tightrope walk between shutting down CGRP fireworks and not turning your coronary arteries into a Chinese finger trap. Fascinating how sumatriptan’s half-life is basically a sprint while frovatriptan’s just chilling like a slow jazz record. But let’s be real-most of us don’t have the luxury of timing our migraines like a NASA launch. We take it when the pain hits like a freight train, aura or no aura. The 20-minute window? More like a myth whispered in neurology conferences while ER docs are busy untangling serotonin syndrome nightmares.
Hayley Ash
So let me get this straight-you’re telling me the only reason triptans work is because they constrict blood vessels like a medieval torture device? And people call this medicine? I’ve had chest tightness so bad I thought I was dying, and the doctor just shrugged and said ‘it’s normal.’ Normal? My dad died of a heart attack at 52. Thanks for the reassurance, science.
Henry Ward
You people are so naive. Triptans are a gateway drug to MOH. You think you’re treating migraines but you’re just training your brain to scream louder every time. I’ve seen patients on 15 triptans a month-then they wonder why they’re in constant pain. It’s not the migraine. It’s the damn medication. Stop treating symptoms like they’re a buffet. You’re not entitled to relief just because you’re in pain. Get a therapist. Learn to breathe. Maybe your pain isn’t biological-it’s emotional.
henry mateo
hey i just wanted to say i took rizatriptan last week and it worked great but i felt super dizzy and my tongue felt weird like metal? is that normal? also i took it with ibuprofen cause my head felt like it was gonna explode and it helped a lot. sorry for the typos im typing on my phone while lying down lol
Kunal Karakoti
There’s a quiet irony in how we treat migraines as a malfunction to be suppressed, rather than a signal from a body that’s been pushed beyond its limits. Triptans are a band-aid on a ruptured dam. We optimize dosing schedules, compare half-lives, and track response rates-but never ask why the dam ruptured in the first place. Sleep? Stress? Gut microbiome? Light sensitivity? We’ve turned neurology into a pharmacological arms race while ignoring the ecosystem that birthed the storm.
Kelly Gerrard
Thank you for this comprehensive and scientifically grounded overview. As a healthcare professional, I cannot emphasize enough the importance of adhering to the 10-day monthly limit. Medication-overuse headache is a silent epidemic. Please do not self-medicate. Consult your neurologist. Your brain deserves better than trial-and-error. Safety first. Always.
Glendon Cone
Just had a 3-day migraine and tried eletriptan for the first time. 90% better in 45 mins 🤯. Also, the chest tightness? Felt like someone hugged me too hard. Lasted 10 mins. Not fun but not scary. I now carry the ODT version in my purse. Life saver. Also, NSAD combo? Yes please. 💪🧠
Sandeep Mishra
For anyone new to this: don’t panic if one triptan fails. It’s like trying different keys for the same lock. My sister tried six before finding frovatriptan. She’s had 3 migraines in 2 years since. Also, if you’re on an SSRI-don’t assume it’s fine. Talk to your pharmacist. Ask for the serotonin syndrome checklist. Knowledge isn’t power here-it’s survival. And if you’re pregnant? Talk to your OB and neurologist together. Don’t let fear silence your voice.
Joseph Corry
How quaint. We have a 30-year-old class of drugs that work via vasoconstriction, and yet we still treat them as the gold standard. Meanwhile, gepants and ditans-non-vasoconstrictive, non-addictive, safe for cardiac patients-are relegated to ‘last resort’ status because Big Pharma doesn’t profit as much from generics. The real tragedy isn’t migraine-it’s the institutional inertia that prioritizes profit over progress. We’re treating 21st-century pain with 1990s tools because someone’s quarterly report depends on it.
Colin L
I’ve been on triptans since I was 19 and now I’m 47 and I’ve had three heart palpitations that sent me to the ER and they always say it’s just the triptan and I’ve had two strokes in my family and my doctor says I’m fine because I’m not hypertensive but I’m not sure I believe him anymore and I’ve been taking them with NSAIDs for 18 years and now I have kidney stones and I think it’s from the naproxen and I don’t know what to do anymore because I can’t function without them and I’ve tried everything else and I’m tired of being told I’m overreacting and I just want to sleep without the pain screaming through my skull like a banshee and I don’t know if I’m brave or stupid for still taking them but I don’t think I have a choice anymore
kelly tracy
So you’re telling me the only reason triptans work is because they’re vasoconstrictors? And you’re calling this medicine? That’s not treatment-that’s chemical warfare on your own body. I’ve had migraines since I was 12. I’ve tried everything. I’ve had 12 ER visits. I’ve been told I’m ‘too sensitive.’ I’ve been called a hypochondriac. And now you want me to trust a drug that makes my chest feel like it’s being crushed by a hydraulic press? No. I’m done. I’m going to try CBD oil. And if I die, at least I’ll die on my own terms. Not yours.