Every year, more than 90% of prescriptions filled in the U.S. are for generic drugs. They’re cheaper, widely available, and trusted. But behind that reliability is a fragile system on the brink. As of April 2025, there were 270 active drug shortages in the U.S.-and nearly all of them involve generics. These aren’t rare glitches. They’re systemic failures that put patients at risk every single day.
Why Generic Drugs Are the Weakest Link
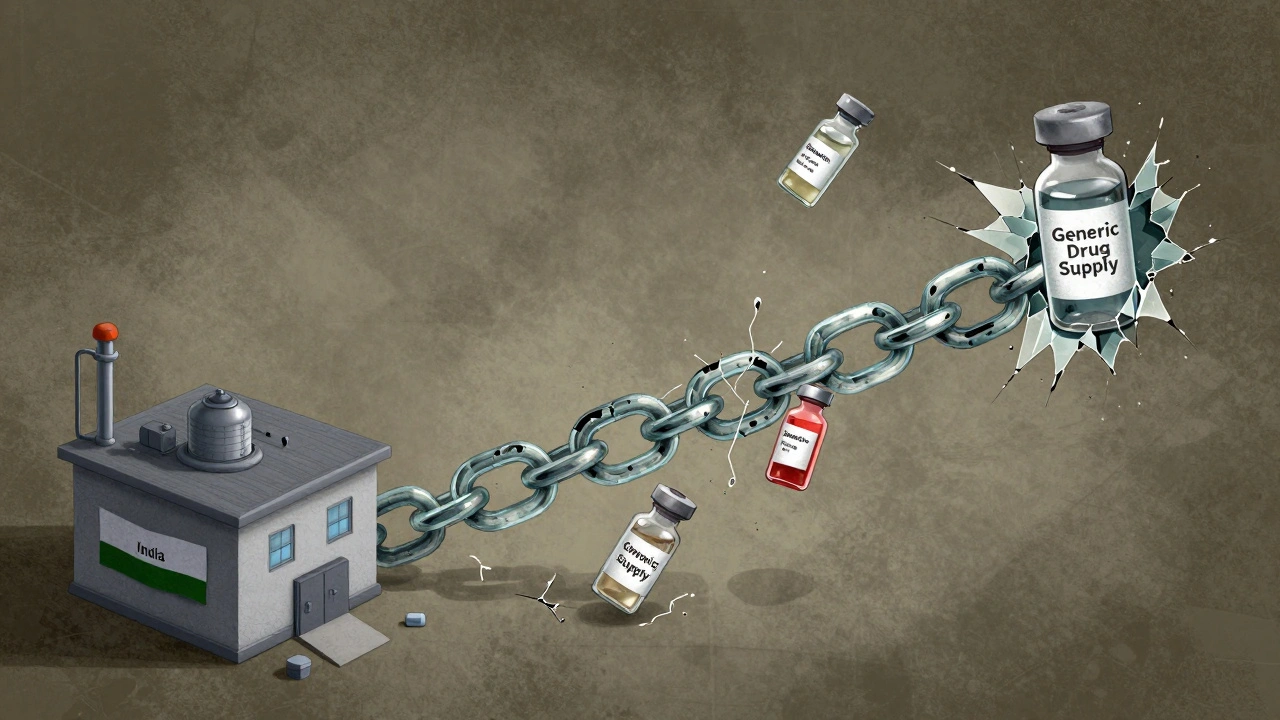
Generic drugs make up 90% of prescriptions but only 13.1% of total drug spending. That’s not a bug-it’s the business model. Manufacturers compete on price, not quality. The result? Thin profit margins. A single vial of epinephrine might cost $2. A bag of IV saline? Less than $1. When you’re making pennies per unit, there’s no room for error, no budget for backups, and no incentive to invest in better equipment or extra inventory. Compare that to brand-name drugs. Companies like Pfizer or Merck spend billions on R&D and charge hundreds or thousands per dose. They can afford multiple suppliers, global warehouses, and quality control teams. Generic manufacturers? They rely on one factory in India, one supplier of active ingredients in China, and one shipping route. Break one link, and the whole chain collapses.The Geography of Risk
Less than 30% of the active pharmaceutical ingredients (APIs) used in U.S. drugs are made here. About 40% come from China. Another 25-30% come from India. These aren’t just distant factories-they’re the backbone of your medicine. In 2023, a tornado destroyed a Pfizer plant in Kentucky. It didn’t make brand-name drugs. It made generic sterile injectables: antibiotics, pain meds, and chemotherapy drugs. Fifteen medications vanished overnight. Hospitals scrambled. Patients delayed treatment. In 2024, the FDA shut down a plant in India producing cisplatin, a critical chemotherapy drug. The reason? Repeated quality violations. No recalls. No warnings. Just a sudden, nationwide shortage. Patients with ovarian and testicular cancer had to wait weeks for alternatives-or none at all. The problem isn’t just natural disasters or bad inspections. It’s concentration. For many older generics, only one or two manufacturers still make them. One plant. One country. One supply line. That’s not a supply chain. It’s a single point of failure.Sterile Injectables: The Most Vulnerable
Not all generics are equal. Sterile injectables-IV fluids, antibiotics, anesthetics, chemotherapy drugs-are the most likely to go short. Why? They’re hard to make. Producing a sterile injection requires clean rooms, specialized equipment, and months of testing. A single speck of dust can ruin a batch. These facilities cost millions to build and maintain. Few companies want to invest in them when they can’t charge more than $5 per vial. According to the USP Annual Drug Shortage Report, sterile injectables account for over 60% of all current shortages. Epinephrine. Heparin. Doxycycline. Vancomycin. These aren’t niche drugs. They’re essentials. Used in emergency rooms, ICUs, and cancer centers. When they’re gone, doctors improvise. And improvising with medicine can kill.
Who Pays the Price?
Hospitals don’t just lose inventory-they lose time. One hospital pharmacist told Pharmacy Times they spend 20-30% of their workweek just tracking down alternatives. Compounding drugs by hand. Calling suppliers. Negotiating with insurers. All while patients wait. Doctors are forced to switch treatments. A patient on a stable dose of generic metformin gets a different brand. Suddenly, their blood sugar spikes. A cancer patient gets a substitute chemo drug with different side effects. A mother waiting for her child’s antibiotic gets a delay. Surgery gets canceled. ICU beds fill up with preventable complications. The American College of Physicians found that shortages hit internal medicine and subspecialties hardest. Diabetics. Cancer patients. ICU patients. People who can’t afford to wait. These aren’t abstract statistics. They’re real people whose care is being rationed because a factory in China had a power outage.Why Tariffs Won’t Fix This
Some politicians propose tariffs on imported drugs-50%, even 200%-to force manufacturing back to the U.S. It sounds simple. But it’s dangerous. Tariffs raise the cost of APIs. That raises the cost of generics. That makes them even less profitable. Manufacturers might quit the market entirely. Shortages get worse. CSIS and the University of Wisconsin School of Pharmacy both warn that tariffs could trigger a new wave of shortages. The same drugs that are already scarce-epinephrine, insulin, heparin-could become unaffordable or unavailable. The people who need them most? They’re the ones who can’t pay more. Rebuilding domestic manufacturing would take 5-7 years and $20-30 billion. Even then, it wouldn’t solve the core problem: low prices. You can’t make a $1 vial of saline profitably in Ohio if you’re competing with a factory in Mumbai that pays workers a fraction of the wage.
What’s Actually Being Done?
There are proposals. The American Hospital Association supports S.2062, which would require manufacturers to keep six months of stock for critical generics. The Strategic National Stockpile could be expanded to include more sterile injectables. Some lawmakers want mandatory labeling so patients know if their drug was made in China or India. But implementation is slow. Federal agencies like the FDA have fewer inspectors. The Department of Health and Human Services has lost staff. Regulatory oversight is shrinking just when it’s needed most. The Association of Accessible Medicines is pushing for public-private partnerships to support manufacturers of high-risk generics. But without price adjustments or guaranteed minimum orders, companies won’t take the risk.The Real Solution Isn’t Political-It’s Economic
There’s no magic fix. No quick policy tweak. The only way to stop these shortages is to make it profitable to make these drugs. That means:- Guaranteed minimum prices for critical generics-enough to cover quality production and inventory.
- Government contracts for essential drugs, like those used in hospitals and emergency response.
- Incentives for multiple manufacturers to enter the market for high-risk drugs.
- Transparency in sourcing-so we know where APIs come from and can spot risks early.
What Patients and Providers Can Do
You can’t fix the supply chain alone. But you can stay informed. - Ask your pharmacist: Is this generic made in the U.S., India, or China? Most don’t know-but they can check. - If your medication is suddenly unavailable, ask if there’s a therapeutically equivalent alternative. - Report shortages to the FDA’s Drug Shortages Program. Your input helps track trends. - Support policies that prioritize patient access over low-cost procurement. This isn’t about blaming manufacturers or countries. It’s about recognizing that medicine shouldn’t be treated like a commodity. When your life depends on a $1 vial, the price shouldn’t be the only thing that matters.Why are generic drug shortages getting worse?
Generic drug shortages are worsening because manufacturers operate on razor-thin profit margins. With prices fixed by competitive bidding, companies can’t afford to invest in backup suppliers, quality improvements, or inventory buffers. When one factory shuts down-due to a natural disaster, quality violation, or geopolitical issue-there’s often no one else to fill the gap. The system was built for low cost, not resilience.
Are all generic drugs at risk of shortage?
No. Oral pills like metformin or lisinopril are less likely to run out because they’re easier and cheaper to produce. The biggest risks are sterile injectables-IV antibiotics, chemotherapy drugs, and emergency medications like epinephrine. These require complex, expensive manufacturing and are often made by only one or two companies.
Can I trust generics made in China or India?
The FDA inspects foreign facilities, but inspections are infrequent and understaffed. Many manufacturers meet standards, but past violations-including contamination and falsified records-have led to shortages. The issue isn’t nationality-it’s oversight. A factory in Ohio could fail just as easily as one in Hyderabad. What matters is consistent quality control, not where it’s made.
Do pharmaceutical tariffs help solve shortages?
No. Tariffs raise the cost of active ingredients, which increases the price of generics. But since generic prices are set by competition, manufacturers can’t raise their prices to cover the cost. The result? They quit making the drug. Shortages get worse. Experts from CSIS and the University of Wisconsin warn that tariffs could trigger more disruptions than they prevent.
How long will these shortages last?
Without major policy changes, shortages will continue. The number of active shortages has been rising since 2014 and hit 323 in early 2024-the highest on record. Even if new factories open, it takes 5-7 years to build and certify them. Meaningful improvement requires coordinated action: better pricing, guaranteed demand, and stronger oversight-not just more inspections.

Harriet Wollaston
I’ve had to switch my mom’s insulin brand three times in the last year because of shortages. She’s 72, diabetic, and terrified every time her prescription doesn’t come in. It’s not just inconvenient-it’s life or death. I wish more people realized these aren’t ‘just pills’-they’re lifelines.
My pharmacist says she spends half her day playing phone tag with suppliers. That’s time she could be counseling patients. We’re treating medicine like toilet paper now.
Lauren Scrima
Oh, so now we’re supposed to pay more… for the same drug? Brilliant. Let’s just throw money at the problem like it’s a Netflix subscription. 🙄
Meanwhile, the factory in India? Still churning out 500 million vials a year. The problem isn’t the country-it’s the greed of middlemen and the FDA’s ‘inspect once, trust forever’ policy.
nina nakamura
The real issue is the FDA is a broken agency that hasn’t updated its inspection protocols since 2008 and still relies on paper logs from foreign plants. The system is designed to fail. No one wants to fix it because the lobbyists for big pharma are richer than your entire town. Stop blaming China. Blame the regulators who let this happen.
Hamza Laassili
AMERICA IS WEAK!! WE LET CHINA AND INDIA MAKE OUR MEDS?!?!?! WE GOTTA BRING IT HOME!! MAKE IT IN OHIO!! WE’RE THE LAND OF THE FREE AND THE HOME OF THE BRAVE!! WHO’S WITH ME?!?!!??!??!?!
Constantine Vigderman
Guys… I just talked to my cousin who works at a hospital in Ohio. They had to use saline bags from a 2019 batch because the new ones didn’t arrive. I mean… 2019? 😳
But here’s the thing-we CAN fix this! Let’s fund domestic API plants, pay manufacturers fairly, and make transparency mandatory. We’ve got the tech. We’ve got the will. We just need the guts to stop treating medicine like a commodity.
Let’s do this 💪🩺🇺🇸
Jamie Clark
Capitalism doesn’t care if you die. It only cares if you pay. The system isn’t broken-it’s working exactly as designed. Profit maximization at the expense of human life is the entire business model. You can’t reform a machine built to exploit scarcity. You have to burn it down and start over.
Universal healthcare isn’t a luxury. It’s the only thing that can force manufacturers to prioritize survival over spreadsheets.
Jennifer Taylor
Okay but what if this is ALL A SETUP? 🤔
What if the FDA and big pharma are working together to create fake shortages so they can push us toward patented drugs? I read a whistleblower report from 2023-some guy said the FDA shut down Indian plants on purpose to make room for new ‘premium generics’ that cost 10x more.
And don’t get me started on the microchips they’re putting in the vials… they track your blood sugar. I swear I felt a buzz when I took my metformin last week. 👁️👄👁️
Someone’s watching. Someone’s always watching.
John Fred
TL;DR: We need a public-private partnership to fund critical generic manufacturers with guaranteed volume contracts + price floors. Think of it like the Defense Production Act for medicine. 🚨
Also-FDA needs more inspectors. Like, 3x more. And they need real-time supply chain dashboards. No more waiting 6 months to find out a plant shut down.
And yes-this is solvable. We just need political will. 💡💊