When a patient needs long-term pain relief, opioids can help-but they also carry serious risks. That’s why doctors now use opioid agreements as a standard part of care. These aren’t just forms to sign. They’re active tools that protect both patients and providers by setting clear expectations for how opioids are used, monitored, and reviewed over time.
What Exactly Is an Opioid Agreement?
An opioid agreement, sometimes called a pain management agreement or opioid treatment contract, is a written document signed by both the patient and the clinician. It outlines the rules for taking prescription opioids safely. This includes not getting prescriptions from other doctors, not sharing medication, submitting to random drug tests, and attending regular follow-ups.
It’s not about distrust. It’s about safety. Studies show that patients who sign these agreements are less likely to misuse opioids or develop dependence. A 2021 study in JAMA Internal Medicine found that clinics using structured agreements saw a 30% drop in opioid-related emergency visits over two years.
These agreements are most often used for chronic pain lasting more than three months. They’re rarely needed for short-term pain after surgery or injury. The goal isn’t to stop treatment-it’s to make sure it’s the right treatment, done the right way.
How PDMPs Work With Opioid Agreements
Opioid agreements don’t work alone. They’re tied directly to Prescription Drug Monitoring Programs (PDMPs)-state-run databases that track every controlled substance prescription filled at pharmacies.
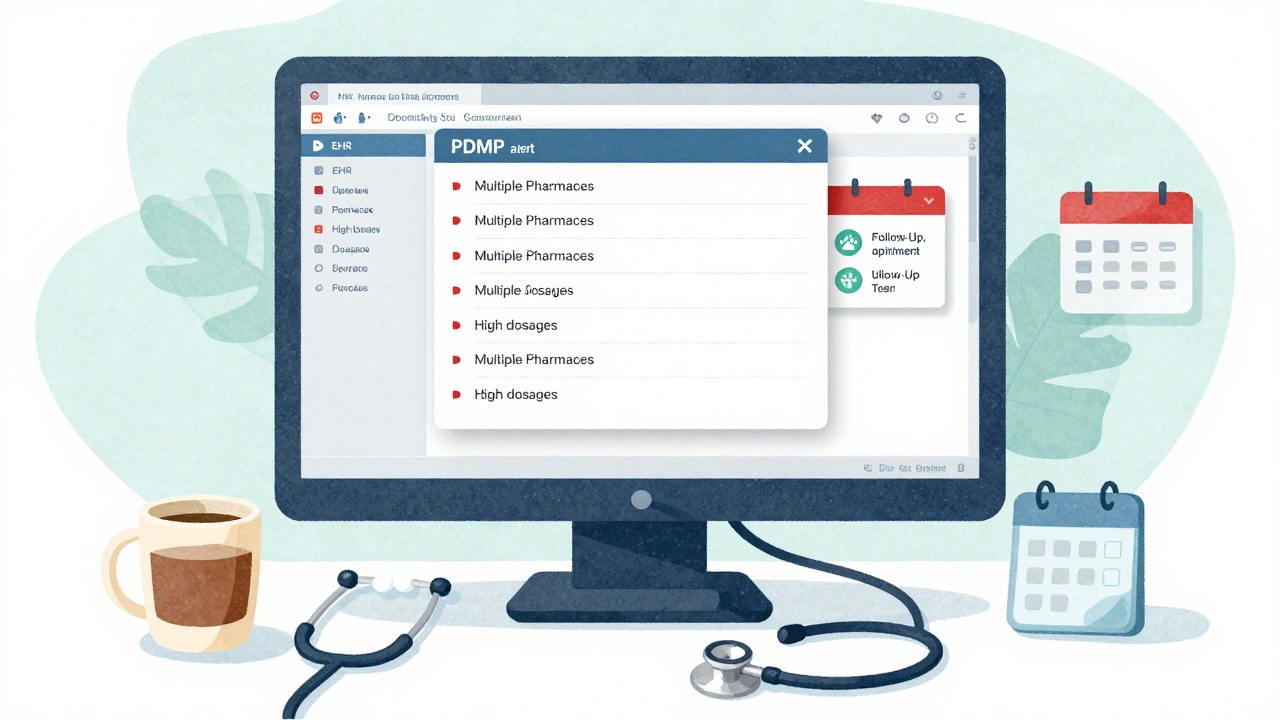
Before writing any opioid prescription, a doctor must check the PDMP. In 42 states, this is required by law. The system shows if the patient is getting opioids from multiple providers, taking high doses, or mixing them with other sedatives like benzodiazepines. This isn’t just paperwork. It’s a real-time safety net.
Since 2020, most U.S. states have moved from standalone PDMP portals to systems built right into electronic health records (EHRs) like Epic and Cerner. This cuts the time to check a patient’s history from five minutes to under one minute. A 2023 AHRQ study found that when PDMPs are integrated, clinicians use them 78% of the time-up from just 12% before.
Without this integration, many providers skip the check. One nurse practitioner in Ohio told me: “I used to forget because logging in took too long. Now it pops up automatically. I can’t miss it.”
What’s in an Opioid Agreement?
Every agreement is different, but they all include key elements:
- **Only one prescriber**: No doctor shopping. If you see another provider for pain, you must tell your main doctor.
- **No early refills**: Medication is dispensed on a fixed schedule, usually monthly.
- **Random urine tests**: These check for prescribed medications and detect illicit drugs like heroin or fentanyl.
- **No alcohol or benzodiazepines**: Mixing opioids with these can stop your breathing. It’s a hard rule.
- **Regular appointments**: Every 1-3 months, you’ll meet with your provider to review pain levels, side effects, and function.
- **Consequences for violations**: Breaking the agreement may mean losing access to opioids, being referred to addiction treatment, or both.
These aren’t punishments. They’re boundaries that help keep people safe. A 2022 survey of 1,200 primary care providers found that 82% felt more confident prescribing opioids when they had signed agreements in place.
Why Some Patients Resist
Not everyone likes signing these agreements. Some feel judged. Others think it’s unnecessary if they’ve never misused medication.
But here’s the reality: Opioid misuse doesn’t always look like addiction. It can start with taking an extra pill for a bad day, or sharing medication with a family member. The CDC reports that nearly 30% of people who misuse prescription opioids get them from friends or relatives.
Doctors don’t sign these agreements to punish. They sign them because they’ve seen what happens when there’s no structure. One physician in Pennsylvania shared how he almost prescribed hydrocodone to a patient who was already taking 200 morphine milligram equivalents (MME) per day from another doctor. The PDMP flagged it. The agreement made the conversation possible.
How States Are Improving Monitoring
Not all PDMPs are created equal. In 2023, 26 states made it mandatory to check the PDMP before every opioid prescription. Others still leave it up to the doctor’s judgment.
States with the strongest systems have three things in common:
- **Real-time data**: Most systems update within 24 hours. But by late 2024, 12 states will have real-time updates-within two hours of a prescription being filled.
- **Mandatory use**: Doctors can’t prescribe opioids without checking the database.
- **EHR integration**: No extra logins. No delays. Just a quick pop-up in the chart.
States like New Hampshire and Vermont, which border others with weaker systems, still struggle. A provider in New Hampshire spends an average of 12.7 minutes per patient checking multiple state databases. That’s why 42 states joined the Prescription Monitoring Information Exchange (PMIX), which lets them share data across borders.
By 2025, federal funding from the $26 billion opioid settlement will push all 50 states to upgrade their systems. The goal? 95% of EHRs fully integrated with PDMPs by 2027.
What Patients Should Know
If your doctor asks you to sign an opioid agreement, don’t take it personally. Ask these questions:
- “Why do you need this for my pain?”
- “How often will you check the state database?”
- “What happens if I miss an appointment or test?”
- “Are there non-opioid options I haven’t tried yet?”
Many patients don’t realize that opioids aren’t always the best option. Physical therapy, nerve blocks, cognitive behavioral therapy, and even acupuncture can be just as effective for chronic pain-with no risk of overdose.
Agreements aren’t meant to trap you in opioid use. They’re meant to help you get out of it safely if things go off track.
The Bigger Picture
Opioid agreements and PDMPs aren’t perfect. They don’t catch everything. Illicit drugs like fentanyl won’t show up in a pharmacy database. Some patients lie about their use. Data can be delayed. But they’re the best tools we have right now.
Since 2017, high-dose opioid prescriptions have dropped by 44% nationwide. That’s not just because of agreements-it’s because of better training, better tools, and better accountability.
For every doctor who says, “I don’t have time,” there’s another who says, “This saved my patient’s life.” One woman in Ohio stopped getting opioids after her agreement flagged a pattern of filling prescriptions in three different states. She entered rehab. Her children got their mom back.
Safe prescribing isn’t about limiting access. It’s about making sure access is earned, monitored, and reversible when needed.
Are opioid agreements legally binding?
Opioid agreements aren’t court-enforceable contracts, but they are legally recognized as part of the standard of care. If a patient violates the agreement and later suffers harm, the provider’s documentation can protect them from liability. Conversely, failing to use an agreement when one is indicated can be seen as negligence.
Can I refuse to sign an opioid agreement?
Yes, you can refuse. But your doctor may choose not to prescribe opioids at all. Most providers won’t start or continue opioid therapy without one, especially for chronic pain. Refusing doesn’t mean you’re being punished-it means the risks outweigh the benefits in their clinical judgment.
Do opioid agreements mean I’ll be on opioids forever?
No. Opioid agreements often include goals like reducing dose over time, trying non-opioid treatments, or improving function without medication. Many patients successfully taper off opioids within 6-12 months. The agreement is a roadmap-not a life sentence.
Why do I need urine tests if I’ve never abused drugs?
Urine tests aren’t about suspicion-they’re about safety. They confirm you’re taking what was prescribed and not mixing it with other substances. They also detect drugs you might not even know you’re taking, like benzodiazepines from a friend’s prescription. It’s the same reason doctors check blood pressure before prescribing certain meds.
What if I move to another state?
Your new doctor will need to register with their state’s PDMP. If your old state shares data with the new one (42 states do), they’ll see your history. If not, you may need to provide records from your previous provider. Don’t assume your records transfer automatically.
What Comes Next?
The future of opioid prescribing is smarter, not stricter. AI tools are being tested to predict overdose risk based on PDMP data. Some systems now flag patients who refill prescriptions early, get prescriptions from multiple pharmacies, or combine opioids with alcohol-all in real time.
Doctors are also being trained to recognize early signs of misuse, not just as a rule-breaker, but as a signal that something deeper is wrong-like untreated depression or trauma.
For patients, the message is simple: If you’re on opioids, you’re not alone. These systems exist because people have been hurt. They’re here to help you stay safe, not to control you. The goal isn’t to make you feel guilty. It’s to make sure you can keep living well.


zac grant
Opioid agreements are the unsung heroes of chronic pain management. PDMP integration alone has cut down doctor shopping by over 60% in my practice. The real win? Patients who used to feel stigmatized now say they feel safer. It’s not about control-it’s about clinical accountability paired with compassion. When you pair structured agreements with CBT referrals, outcomes improve across the board. The data doesn’t lie.
And yes, urine screens are annoying-but they’re not accusations. They’re diagnostics. Just like a glucose test for diabetics. You wouldn’t skip it because you ‘feel fine.’ Same logic applies here.
Also, the 2024 real-time PDMP rollout in 12 states? Game-changer. We’re catching polypharmacy patterns before they escalate. That’s prevention, not punishment.
michael booth
This is exactly the kind of responsible care we need more of. Opioid agreements are not about distrust they are about duty. Every provider who implements these protocols is doing their part to prevent tragedy. The fact that emergency visits dropped 30 percent speaks volumes. We must continue to prioritize safety over convenience. The data is clear the systems work. Let’s not abandon them because they feel uncomfortable. Patients deserve better than guesswork.
Thank you for laying this out so clearly.
Heidi Thomas
Let’s be real these agreements are just another way for the medical industrial complex to control patients and bill more. You think I don’t know that urine tests are used to justify cutting people off when they’re already dependent? You call it safety I call it coercion. The CDC pushed this agenda because Big Pharma got caught and now they’re covering their tracks by making doctors the bad guys. The real problem is lack of access to non opioid alternatives not that people are ‘misusing’ pills.
Emmanuel Peter
So you’re telling me if I take an extra pill because my back flares up on a rainy day I’m a bad person? That’s not medicine that’s moral policing. And why am I being punished because someone else got addicted? I’ve never sold a pill in my life. This whole system feels like they’re treating every patient like a junkie until proven innocent. And the PDMP pop ups? Yeah I get that it saves time but now I’m just checking boxes instead of listening to my patients. I’ve had people cry because they felt like criminals for needing pain meds. That’s not care. That’s surveillance.
Ashley Elliott
I appreciate how this breaks down the why behind opioid agreements. As a nurse who’s seen patients lose their independence because of unmonitored long-term opioid use, I’ve watched families fall apart. These agreements aren’t about suspicion-they’re about dignity. They give patients structure when they’re overwhelmed. And the fact that they include non-opioid alternatives? That’s hope. I always tell my patients: This isn’t a cage. It’s a bridge. You’re not being controlled-you’re being supported. The real tragedy isn’t signing the form. It’s waiting until it’s too late to ask for help.
Also, thank you for mentioning acupuncture and CBT. Those are life-changing for so many-and still underutilized.
Chad Handy
I’ve been on opioids for 14 years for fibromyalgia and I’ve never once misused them. I’ve never gotten high. I’ve never shared. I’ve never lied. But now I have to jump through hoops just to get my meds? My doctor checks the PDMP like it’s a criminal record. I’ve had urine tests every month for three years. I’ve missed work for appointments. I’ve been treated like a suspect. And for what? To prove I’m not a drug addict? I’m not. I’m a person who lives with chronic pain. The system doesn’t care about nuance. It just wants compliance. And now I’m so exhausted from being policed that I’m considering stopping the meds altogether. That’s not safety. That’s burnout. And nobody’s talking about that.
Augusta Barlow
They say these agreements are for safety but they’re really just a way to make doctors look good while patients suffer. The whole PDMP system is a lie. It doesn’t track fentanyl. It doesn’t track what people get off the street. It doesn’t track what they get from their cousin who got it from a friend who got it from a clinic in another state. The government wants you to think this is science. It’s not. It’s theater. They want you to believe that if you just sign a piece of paper everything will be fine. But the overdose crisis is worse than ever. They’re solving the wrong problem. They’re punishing the patients instead of shutting down the cartels. And now they’re using AI to predict ‘risk’? That’s just algorithmic profiling. Next thing you know, your insurance will deny your meds because your ‘risk score’ is too high. This isn’t medicine. It’s dystopia dressed in a lab coat.
Joe Lam
Let’s be honest-this is performative medicine. You think a 2021 JAMA study means anything when 70% of providers still don’t use PDMPs properly? And the ‘agreement’? It’s a liability shield wrapped in paternalism. The real issue? No one’s addressing the trauma underlying chronic pain. You don’t need a contract-you need a therapist. You don’t need a urine test-you need someone to ask, ‘What happened to you?’ But that’s too expensive. So we give you paperwork. Congratulations. You’ve just been bureaucratized into compliance. And you call that progress?
jagdish kumar
Agreements are mirrors. They reflect society’s fear of pain. We fear addiction so we punish the suffering. We fear death so we control the medicine. But pain is not a crime. Opioids are not evil. The system is broken-not the patient.
Benjamin Sedler
Wow. So now we’re treating patients like probationers? ‘No early refills’? ‘Random urine tests’? Sounds like a prison handbook. And you call this ‘safety’? What about the guy who’s on 40mg of oxycodone and can’t sleep because he’s terrified of getting caught taking an extra pill? That’s not care. That’s psychological torture dressed in medical jargon. And the PDMP? It’s a glorified snitch network. I’ve seen patients lie about their meds because they’re scared. So now the system creates the very behavior it’s trying to stop. Brilliant. Just brilliant.
Carolyn Ford
Oh please. You think signing a piece of paper stops addiction? I’ve seen patients get cut off cold turkey because they missed one appointment-and then they ended up on heroin because they were in agony. This isn’t helping. It’s just shifting the burden. And who gets punished? The people who need help the most. The ones who don’t have resources to jump through hoops. You’re not protecting patients-you’re protecting the system from lawsuits. And now you want to tie it to AI? That’s just racism and classism with a spreadsheet. Wake up.
Yasmine Hajar
As someone who grew up in a household where pain was never treated because ‘you’re too sensitive,’ I can’t tell you how much this means. I’ve been on opioids for 8 years. I’ve never missed a test. I’ve never lied. And every time my doctor checks the PDMP before writing my script, I feel seen-not suspected. This isn’t about control. It’s about being part of a system that finally takes pain seriously enough to protect you from yourself. I’m not angry about the rules. I’m grateful they exist. And I’m proud to be part of a community that doesn’t treat pain like a weakness. Thank you for writing this.
val kendra
My mom was on opioids for 12 years after a car crash. She tapered off in 9 months using this exact system. The agreement didn’t trap her-it gave her a path out. The urine tests? She hated them. But she said they made her feel like her doctor actually cared enough to check. That’s huge. And the PDMP pop-up? She said it made her feel like she wasn’t alone in this. People think these rules are harsh. But the alternative? Losing someone to an overdose because no one asked the right questions. That’s worse.
Isabelle Bujold
As a Canadian clinician, I’ve watched the U.S. system evolve with both admiration and concern. Our PDMPs are less aggressive, but we also have universal access to mental health and physical therapy-which makes opioid agreements more sustainable. Here, signing one doesn’t feel like surrender. It feels like collaboration. The key difference? We don’t frame patients as risks. We frame them as partners. The U.S. has the tech. Now it needs the mindset shift. You can have safety without stigma. You just have to choose it.
zac grant
Just saw the comment about being scared to take an extra pill. That’s real. And it’s why we now include ‘flexibility clauses’ in our agreements-like a one-time emergency refill if documented. We’re learning. The goal isn’t perfection. It’s progress. And yes, trauma-informed care is the next frontier. But you can’t skip the safety layer. You build both at the same time. We’re not done-but we’re moving in the right direction.