Why Sarcopenia in COPD Is More Than Just Weakness
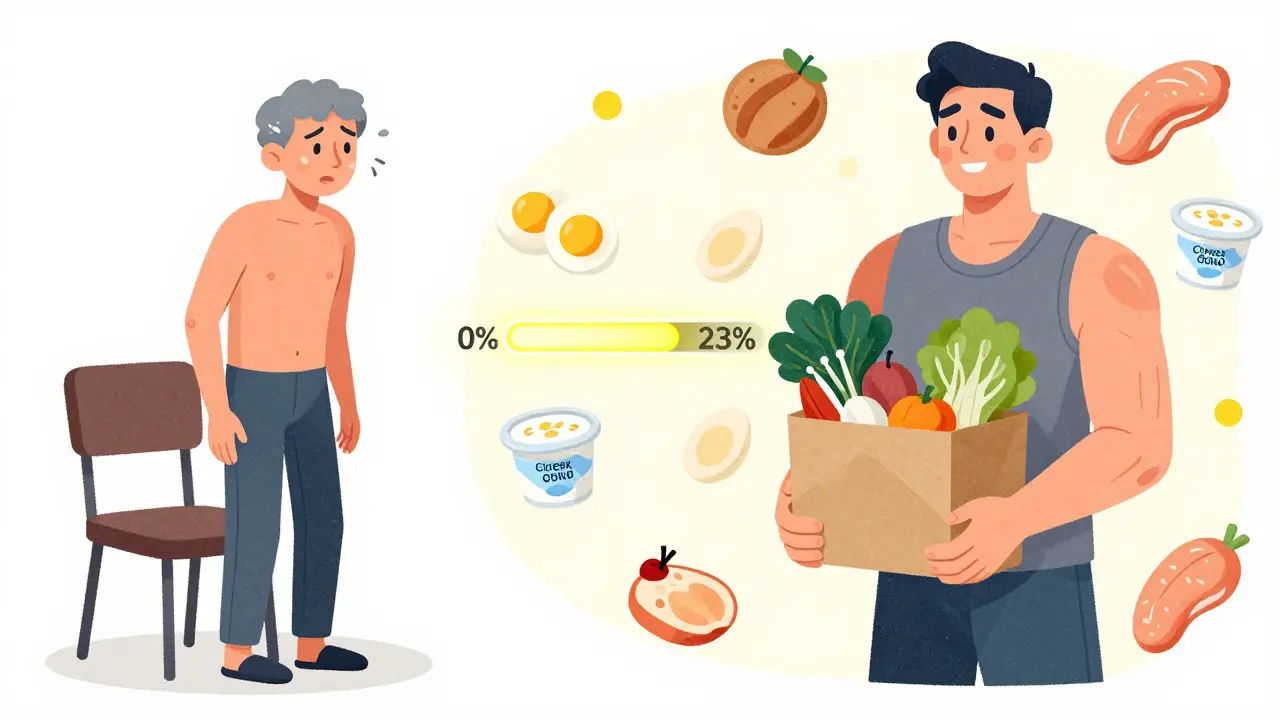
When you have COPD, breathing gets harder. But what most people don’t realize is that your muscles are also breaking down-fast. Sarcopenia, the loss of muscle mass and strength, affects about 22% of people with COPD. That’s more than 1 in 5. And it’s not just about feeling tired. This muscle loss directly lowers your chances of living longer, increases hospital stays, and makes everyday tasks like climbing stairs or carrying groceries nearly impossible.
Unlike normal aging, where muscle slowly fades, sarcopenia in COPD hits harder and faster. Studies show people with COPD lose muscle at 3.2% per year, nearly double the rate of healthy older adults. And it’s not just your legs. The muscles that help you breathe-like the pectoralis major-are often the first to weaken. In fact, 68% of COPD patients show serious atrophy in these upper body muscles, compared to just 22% of healthy peers. This isn’t just weakness. It’s a systemic problem tied to inflammation, low oxygen at night, poor nutrition, and inactivity.
How Doctors Diagnose Sarcopenia in COPD
Most clinics don’t screen for sarcopenia unless you ask. But it’s easy to check. The European Working Group on Sarcopenia in Older People (EWGSOP2) says the first sign is low muscle strength-not muscle size. For men, that means a handgrip strength under 27 kg. For women, under 16 kg. That’s less than a full grocery bag.
Next, they look at muscle quantity. A DEXA scan measures lean mass in your arms and legs. If your appendicular skeletal muscle index is below 7.0 kg/m² (men) or 5.5 kg/m² (women), that’s a red flag. But here’s the catch: in COPD, BMI doesn’t tell the whole story. Many patients are thin but still have low muscle mass. That’s why doctors now use the pectoralis muscle index (PMI)-a CT scan of the chest muscle at the L3 level. A PMI below 1.06 cm²/BMI is a strong indicator of sarcopenia in COPD.
Finally, they test movement. Can you stand up from a chair without using your arms? Can you walk four meters in under 0.8 seconds? If not, your physical performance score is too low. This isn’t just about fitness-it’s about survival. People with all three signs (low strength, low mass, low performance) have up to a 40% higher risk of dying than COPD patients without sarcopenia.
Why Standard Exercise Programs Fail in COPD
You might think: “I’ll just lift weights like everyone else.” But that’s where things go wrong. People with COPD don’t respond to normal resistance training. When they try, 42% need supplemental oxygen just to complete a set. Many quit after one or two sessions because their breathing becomes unbearable.
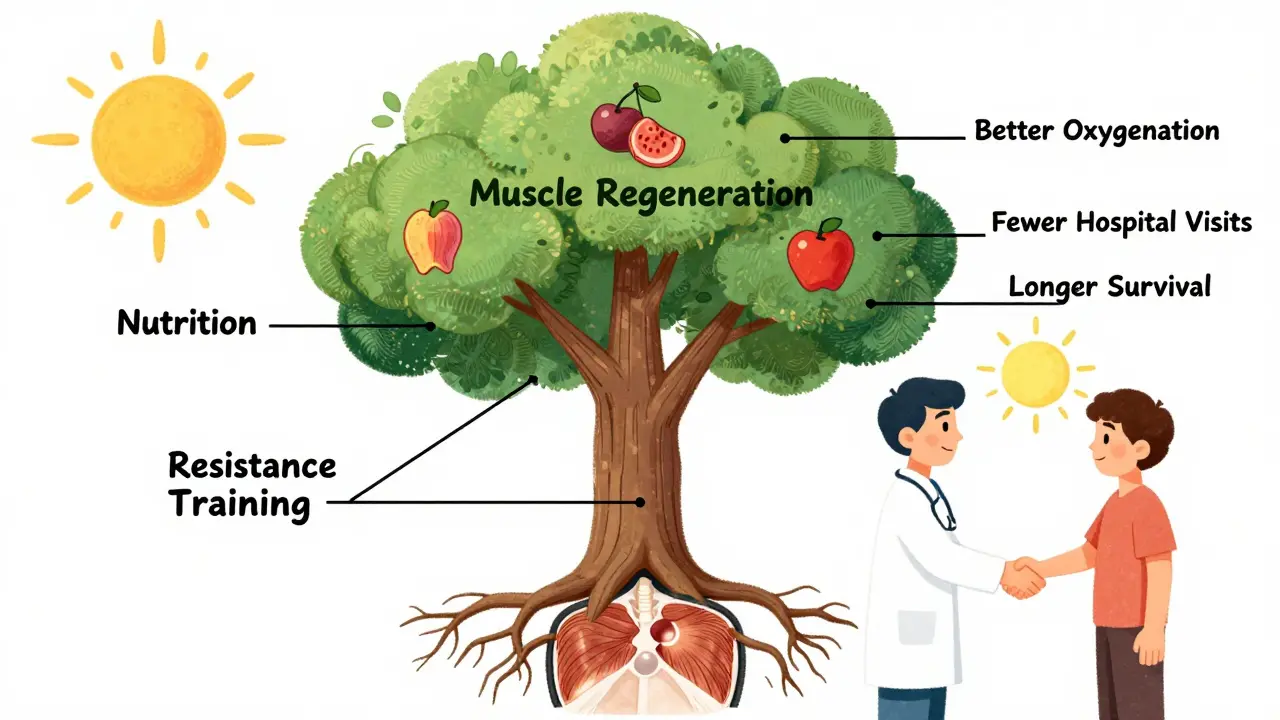
Standard programs start at 60-80% of your one-rep max. That’s too much. The right approach starts at 30-40% of your 1-RM. That’s light-think 1 to 2-pound dumbbells or resistance bands. The goal isn’t to exhaust you. It’s to trigger muscle growth without triggering breathlessness.
Timing matters too. Rest between sets needs to be longer-2 to 3 minutes. This lets your oxygen levels recover. Sessions should be short: 20-30 minutes, 2-3 times a week. Focus on major muscles: legs (seated leg extensions), arms (bicep curls), chest (wall push-ups), and core (seated marches). Progress slowly. It takes 8 to 12 weeks to see real gains. But when it works, the 6-minute walk distance improves by 23% on average.
What to Eat-And What Not to Eat
Most COPD patients eat too little protein. The average intake? Just 0.9 grams per kilogram of body weight. The recommended amount? 1.2 to 1.5 grams per kg. That’s a 33% gap. And it’s not just about quantity-it’s about timing.
Spread your protein across four meals. That means 0.3 to 0.4 grams per kg per meal. For a 70 kg person, that’s about 21-28 grams of protein per meal. That’s a chicken breast, a cup of Greek yogurt, or two scoops of whey protein.
Leucine is the key amino acid that turns on muscle growth. Most foods don’t have enough. That’s why adding 2.5 to 3.0 grams of leucine per meal helps. Whey protein supplements often contain this naturally. Look for products labeled with “10g leucine per serving.” Studies show this boosts muscle protein synthesis by 37% in COPD patients.
Don’t rely on shakes alone. Real food matters. Eggs, fish, lean meat, cottage cheese, and lentils are all good. Avoid sugary snacks and processed carbs-they fuel inflammation. And if you’re losing appetite (common in advanced COPD), try smaller, more frequent meals. High-calorie, high-protein smoothies with peanut butter, banana, and protein powder can help.
Real People, Real Results
Mary Thompson, 68, has GOLD Stage 3 COPD. For years, she couldn’t carry her purse without stopping to catch her breath. She joined a pulmonary rehab program that combined light resistance bands with protein shakes. After 12 weeks, she could carry groceries again. “I didn’t feel stronger,” she said. “I just didn’t feel like I was going to collapse every time I moved.”
John Peterson, 72, tried the same program but didn’t get oxygen support. “I got so short of breath after three sessions, I quit,” he posted online. His story isn’t rare. Nearly 32% of patients drop out because they weren’t prepared for how hard it feels.
The Cleveland Clinic tracked 78 patients with moderate to severe COPD and sarcopenia. After 16 weeks of supervised training and 1.2 g/kg/day protein, their 6-minute walk distance improved by 23%. Hospital visits dropped. Quality of life scores rose. This isn’t a miracle. It’s science.
What’s New and What’s Coming
In 2024, GOLD (the Global Initiative for Chronic Obstructive Lung Disease) released the first-ever algorithm for managing sarcopenia in COPD. It links nighttime oxygen levels to exercise intensity. If your oxygen drops below 88% for more than 30% of sleep, your training load gets reduced. This is a game-changer.
Researchers are testing new supplements like HMB (beta-hydroxy-beta-methylbutyrate), which helps preserve muscle during inactivity. Early results show 18% better muscle retention compared to placebo. Another drug, PTI-501, a myostatin inhibitor, is in phase 2 trials. It blocks a protein that limits muscle growth. If it works, it could be the first pill specifically for COPD-related muscle loss.
But the biggest shift isn’t a drug or device. It’s awareness. In 2020, only 22% of U.S. rehab centers screened for sarcopenia. Today, it’s 38%. Academic centers are at 67%. Community clinics are still lagging. But the trend is clear: if you have COPD, you need to be checked for muscle loss-and treated for it.
Where to Start Today
- Ask your doctor for a handgrip strength test. It takes 30 seconds and costs nothing.
- Track your protein intake. Use a free app like MyFitnessPal. Aim for 1.2-1.5 g/kg/day. If you’re 70 kg, that’s 84-105 grams daily.
- Start with resistance bands. Sit in a chair. Loop a band around your foot. Gently pull your leg back. Do 10 reps. Rest 2 minutes. Repeat twice. Do this 3 times a week.
- Get oxygen if you need it. If you’re breathless during exercise, ask about using supplemental oxygen during training. It’s not a sign of weakness-it’s a tool.
- Don’t quit during flare-ups. Take a break, but don’t stop. Even light walking or seated arm circles helps. Muscle loss accelerates when you’re inactive.
Sarcopenia in COPD isn’t inevitable. It’s treatable. And the best part? You don’t need a gym. You don’t need expensive gear. You just need to move a little more, eat a little more protein, and ask for help. The science is clear. The results are real. And your body still has the ability to rebuild-if you give it the right support.


Nina Stacey
ive been living with copd for 8 years and i never realized how much my muscles were failing me until i couldnt pick up my grandkids anymore
the part about handgrip strength being the first sign really hit home i had no idea it was that simple to check
i started doing those band exercises from the post and honestly it felt silly at first but after 6 weeks i can carry my grocery bags without stopping
my doctor was shocked i told her i just followed the 30-40% rule and took long rests
its not about lifting heavy its about not passing out
also started eating more protein i used to skip breakfast now i have 2 eggs and a yogurt every morning
the leucine thing sounds weird but i got whey with 10g per scoop and it actually helps me feel less wiped out after
im not cured but im not falling apart anymore and thats something
Kevin Motta Top
23% improvement in 6-minute walk? That’s huge. Simple, science-backed, no magic pills needed.
Alisa Silvia Bila
so many people think copd is just about lungs but this post shows it’s really about the whole body
the fact that chest muscles weaken first is wild i never thought about breathing muscles being part of sarcopenia
also love that it’s not about gym bros lifting heavy just small consistent moves
and protein timing? that’s the secret sauce i wish my doctor told me this 5 years ago
Marsha Jentzsch
STOP RIGHT NOW. I’ve been saying this for YEARS. The government and big pharma are hiding the truth about sarcopenia because they make more money selling inhalers than fixing the real problem - your muscles! They don’t want you to get strong - they want you dependent! And don’t get me started on whey protein - it’s loaded with GMOs and fluoride! I read a study on a blog once that said 92% of supplements are contaminated with rat hair - I’m not kidding! You think your doctor cares? They get kickbacks from Big Pharma! I’ve been taking apple cider vinegar and doing yoga in my basement with no oxygen and I’ve doubled my strength! Just stop trusting the system - and eat more kale! Also - did you know the moon controls inflammation? I’m not joking - check the lunar calendar before you train!
Chris porto
it makes sense that if you cant breathe well your body just stops investing in muscle
its like your body says hey we need oxygen for survival not for lifting dumbbells
so it shuts down the non-essential stuff
and yeah protein timing makes sense too
you cant just dump it all in one meal
its like watering a plant once a week instead of a little every day
the part about oxygen during training? that’s not weakness
its smart adaptation
we need to stop seeing it as failure and start seeing it as part of the plan
Danielle Stewart
to anyone reading this who feels overwhelmed - start with one thing
one protein shake. one set of seated leg extensions. one handgrip test
you don’t have to fix everything today
progress isn’t loud
it’s quiet
it’s showing up when you’re tired
it’s choosing the yogurt over the donut
it’s asking for oxygen even if you feel embarrassed
you’re not behind
you’re just beginning
and that’s more than enough
jessica .
THIS IS A LEFTIST SOCIAL ENGINEERING TACTIC TO MAKE OLD PEOPLE WEAK AND DEPENDENT
THEY WANT YOU TO THINK YOU NEED SUPPLEMENTS AND OXYGEN BECAUSE THEY’RE HIDING THE REAL SOLUTION - JUST PUSH THROUGH AND BE A MAN
MY GRANDPA WALKED 5 MILES TO WORK IN THE 50S WITH A COPD DIAGNOSIS AND NEVER USED A SHAKESPEAREAN OXYGEN TANK
THEY’RE MAKING YOU SOFT TO CONTROL YOU
STOP BUYING INTO THE WOKE MUSCLE LIE
JUST EAT MEAT AND DO PUSH UPS ON THE FLOOR LIKE GOD INTENDED
Ryan van Leent
why do people think this is new info
my grandpa did this in the 80s with soup cans and a chair
they just repackaged it with fancy words and called it science
and now everyone’s acting like they discovered fire
also 1.5g per kg? that’s just common sense
why are we paying for studies to tell us to eat more protein
and why is everyone so shocked that weak muscles make you weak
its like saying water is wet
Sajith Shams
you all are missing the point. the real issue is not protein or bands or oxygen - its the lack of discipline. in india we train with bodyweight since childhood. no machines. no supplements. no excuses. you want strength? you lift your own weight. you want to breathe better? you walk uphill. you want to survive? you stop complaining. the west overcomplicates everything. the solution is simple: move. eat real food. stop watching screens. if you can’t do 10 squats without gasping - you’re lazy. not sick. this post is a distraction. the real enemy is comfort. get up. move. survive. no doctor needed. no study needed. just willpower.