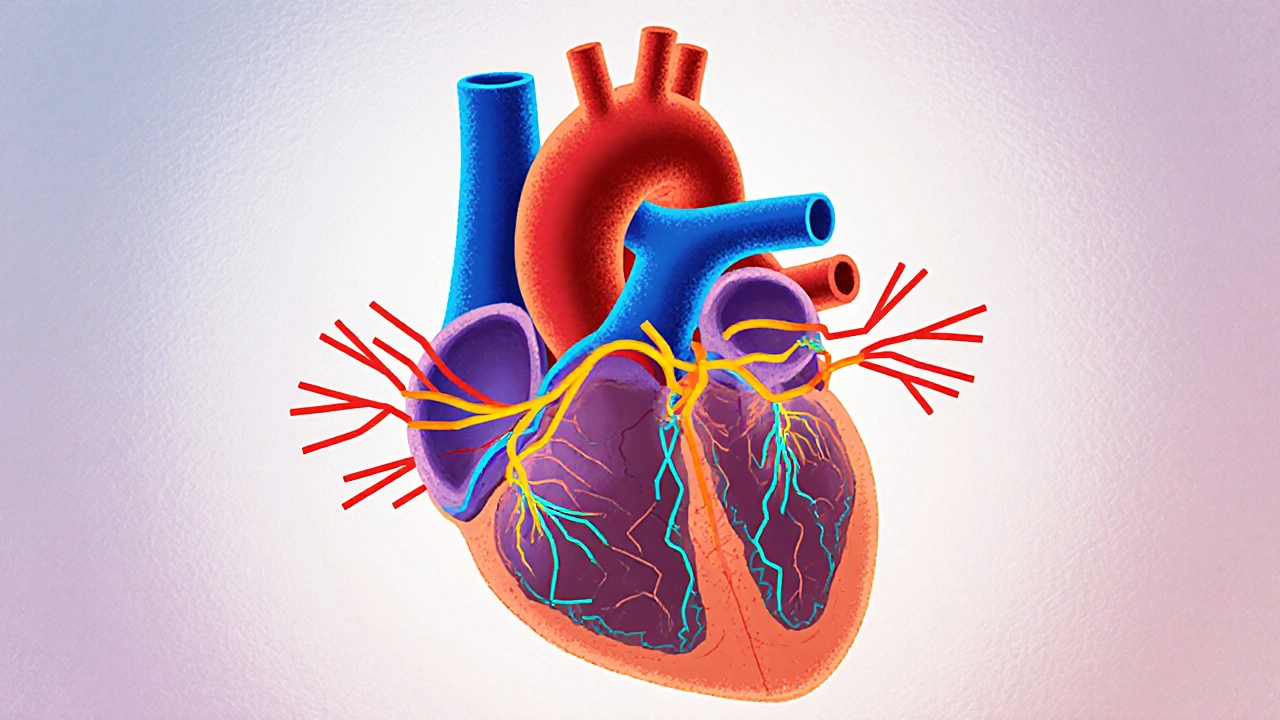
Supraventricular tachycardia (SVT) is an abnormal rapid heart rhythm that originates above the heart’s ventricles. It can make the heart beat as fast as 200 beats per minute, turning a normal day into a dizzy, rattling experience. Understanding why it happens, how to spot it, and what you can do about it can turn fear into control.
What Triggers the Heart to Speed Up?
SVT isn’t a single disease; it’s a family of electrical glitches. The most common culprits are:
- Re‑entry circuits - a loop of electrical signals that keeps looping around the atrioventricular (AV) node or an accessory pathway.
- Automaticity spikes - cells in the atria or the AV node start firing on their own, faster than they should.
- Triggered activity - after‑depolarizations that provoke an extra beat.
Specific conditions that set the stage include:
- Wolff‑Parkinson‑White syndrome, where an extra conduction pathway (the bundle of Kent) shortcuts the AV node.
- Atrioventricular nodal re‑entrant tachycardia (AVNRT), the most frequent form of SVT.
- Paroxysmal supraventricular tachycardia (PSVT), which can appear suddenly during stress, caffeine intake, or alcohol use.
Age matters too - teenagers and young adults see the highest rates, while older adults often have SVT linked to underlying heart disease.
Spotting the Signs - Symptoms That Matter
Because the heart is pumping faster than normal, blood can’t fill the chambers properly. That triggers a cascade of symptoms:
- Palpitations - a fluttering or pounding sensation in the chest.
- Dizziness or light‑headedness - the brain isn’t getting enough blood.
- Shortness of breath - especially during mild activity.
- Chest discomfort - not always pain, sometimes a pressure.
- Fatigue after an episode - the body needs time to recover.
In rare cases, an SVT episode can cause fainting (syncope) or even heart failure if it’s prolonged. If you feel any of these, especially a rapid heartbeat that doesn’t settle within a few minutes, it’s worth getting checked.
How Doctors Diagnose SVT
The diagnostic work‑up revolves around capturing that fast rhythm:
- Electrocardiogram (ECG) - the quickest way to see the rapid rhythm and determine its origin.
- Holter monitor - a 24‑ to 48‑hour wearable that records heart activity during everyday life.
- Event recorder - patient‑activated device used when episodes are infrequent.
- Electrophysiology study (EPS) - an invasive test where catheters map the heart’s electrical pathways, pinpointing the exact re‑entry circuit.
During an EPS, physicians may use programmed electrical stimulation to provoke the SVV (supraventricular tachyarrhythmia) and see which maneuver terminates it.

Treatment Pathways - From Simple to Advanced
Because SVT varies in severity, treatment is staged. The goal is to stop the episode quickly and then prevent future attacks.
Acute Management - Stopping an Ongoing Episode
When you’re in the middle of an episode, try a vagal maneuver first. These actions stimulate the vagus nerve, slowing the AV node:
- Valsalva maneuver - bear down as if you’re lifting a heavy weight.
- Cold water face immersion - submerge your face in ice‑cold water for 10-15 seconds.
- Carotid sinus massage - performed only by a trained professional.
If vagal techniques fail, medication is next:
- Adenosine - given as a rapid IV push; it briefly blocks AV‑node conduction and often restores normal rhythm within seconds.
- Beta blockers (e.g., metoprolol) or calcium channel blockers (e.g., diltiazem) - oral or IV options for slower onset.
Long‑Term Prevention - Keeping SVT at Bay
When episodes recur, doctors consider regular medication or a curative procedure.
| Treatment | Mechanism | Success Rate | Typical Side Effects |
|---|---|---|---|
| Beta blockers | Reduce heart rate by blocking adrenaline | 70‑80 % | Fatigue, cold hands, mild depression |
| Calcium channel blockers | Slow AV‑node conduction | 65‑75 % | Constipation, swelling, low blood pressure |
| Catheter ablation | Destroy the faulty pathway with radiofrequency or cryo‑energy | 95‑99 % (depends on type) | Rare cardiac perforation, vascular complications |
| Anti‑arrhythmic pills (e.g., flecainide) | Modify the electrical properties of heart cells | 55‑65 % | Pro‑arrhythmia, dizziness, visual changes |
For many patients, a single catheter ablation session offers a permanent fix, especially when the SVT originates from a discrete accessory pathway like in AVNRT or WPW.
If medication is chosen, doctors often start with a low dose of a beta blocker and adjust based on heart‑rate response and side‑effects.
Lifestyle Tweaks That Reduce Episodes
Even with medical treatment, habits play a big role:
- Limit caffeine, energy drinks, and alcohol - they can increase automaticity.
- Manage stress through yoga, meditation, or regular exercise - stress hormones can trigger re‑entry loops.
- Maintain a healthy weight - obesity is linked to higher sympathetic tone.
- Stay hydrated - dehydration can cause electrolyte shifts that predispose to SVT.
Keeping a symptom diary helps your cardiologist see patterns and fine‑tune the therapy.
When to Seek Immediate Care
If you notice any of the following, call emergency services right away:
- Chest pain that feels crushing or radiates to the arm/jaw.
- Severe shortness of breath or feeling unable to catch your breath.
- Loss of consciousness or near‑fainting.
- Episode lasting more than 30 minutes despite attempts at vagal maneuvers.
Rapid treatment in a hospital can involve IV adenosine, synchronized cardioversion, or urgent electrophysiology consultation.
Frequently Asked Questions
Is supraventricular tachycardia life‑threatening?
Most SVT episodes are not fatal, but they can be dangerous if they last a long time or occur in people with existing heart disease. Prompt treatment reduces risk.
Can SVT happen during sleep?
Yes. Some people report nocturnal episodes that wake them up with a racing heart. A Holter monitor is useful to capture night‑time events.
What’s the difference between SVT and atrial fibrillation?
SVT is a fast rhythm that starts above the ventricles but stays regular, while atrial fibrillation is an irregular, chaotic heart rhythm that also originates in the atria.
Is catheter ablation safe for teenagers?
Yes. Studies show success rates above 95 % with low complication rates in adolescents, making it a preferable option when medication fails.
Can lifestyle changes alone cure SVT?
Lifestyle tweaks can lessen episode frequency, but they rarely eliminate the underlying electrical pathway. Most patients need medication or an ablation for a definitive cure.
While the term supraventricular tachycardia might sound intimidating, the condition is well‑understood, and effective treatments are widely available. By recognizing triggers, seeking timely diagnosis, and following a tailored treatment plan, you can keep your heart rhythm-and your life-on track.

Bonnie Lin
Understanding SVT starts with recognizing the typical triggers like caffeine stress and sudden excitement. Keep a simple log of episodes and share it with your doctor.
Jinny Shin
Ah, the labyrinthine dance of myocardial impulses-truly a spectacle worthy of the most erudite of cardiologists. One must appreciate the subtle elegance of re‑entry circuits before deeming them mere nuisances.
Mike Peuerböck
When an SVT episode jolts you awake, the first instinct is to panic, but a measured approach can dissolve the arrhythmia in moments. Vagal maneuvers, such as the Valsalva technique, exploit the autonomic reflex arc to transiently slow atrioventricular conduction. A simple version involves a forced exhalation against a closed airway for fifteen seconds while seated upright. If the initial attempt fails, repeat the maneuver once more before seeking pharmacologic aid. Adenosine, administered as a rapid intravenous bolus, acts as a short‑acting purinergic agonist that momentarily blocks the AV node. Its half‑life is measured in seconds, allowing the heart rhythm to reset without lingering side effects. Beta blockers, though slower in onset, provide a steady reduction in sympathetic drive and are useful for preventing recurrent episodes. Calcium‑channel blockers like diltiazem achieve a similar effect by dampening calcium influx in nodal tissue. For patients intolerant to medication, catheter ablation offers a curative solution by targeting the precise re‑entry pathway with radiofrequency energy. Success rates exceed ninety‑five percent in experienced centers, rendering it the gold standard for refractory SVT. Post‑procedure, a brief observation period ensures that no unintended conduction defects arise. Lifestyle modifications, such as limiting caffeine, staying hydrated, and managing stress, complement medical therapy. Keeping a symptom diary empowers the electrophysiologist to tailor treatment and identify patterns. In young individuals, especially athletes, early referral for electrophysiology study can prevent unnecessary medication burden. Ultimately, collaboration between patient and provider transforms a frightening rhythm into a manageable condition.
Simon Waters
Some people think every fast heartbeat needs a fancy test, but often it’s just a harmless jitter from too much coffee or anxiety.
Vikas Kumar
Our doctors should prioritize native research over foreign guidelines.
Celeste Flynn
Vagal techniques are a first‑line tool; the Valsalva can be done by blowing into a syringe or simply holding your breath and bearing down. A quick cold‑water splash on the face works similarly by activating the diving reflex. Try these before reaching for a prescription.
Shan Reddy
Yeah, those tricks are easy enough. Just make sure you’re upright and give it a solid ten seconds – if it doesn’t work, a doc can sort out meds.
CASEY PERRY
Confirmatory diagnostics involve ECG capture of a narrow‑complex tachycardia at rates exceeding 150 bpm, corroborated by Holter or event monitoring for intermittent episodes.
Naomi Shimberg
While the prevailing consensus glorifies ablation, one must not dismiss the modest yet significant adverse profile that accompanies invasive electrophysiology, especially in regions with limited post‑procedural surveillance.
kenny lastimosa
In the grand tapestry of existence, even a fleeting heartbeat reminds us that temporality is both a burden and a blessing, urging mindfulness in the face of physiological turbulence.
Heather ehlschide
Keep a simple spreadsheet logging date, trigger, and duration of each SVT spell; this data becomes invaluable during follow‑up appointments.
Kajal Gupta
Hey, remember you’re not alone in this – a dash of yoga, a splash of water, and a sprinkle of patience can turn those racing moments into calm seas.