Chronic Pain Management: Real‑World Tips to Feel Better
Living with pain that never seems to quit can wear you down. What if you could shave off a few hours of soreness each day with small changes? Below you’ll find easy steps you can start right now, plus a quick rundown of medicines and therapies that actually work for many people.
Everyday habits that cut pain
First off, move a little every day. Even a 10‑minute walk or gentle stretching can keep joints from stiffening and release natural pain‑killing chemicals called endorphins. Try a simple routine: neck rolls, shoulder shrugs, ankle circles, then a short walk around the block. Consistency beats intensity – doing a little each day beats a marathon once a month.
Sleep matters more than you think. Poor sleep spikes pain signals, creating a vicious loop. Aim for 7‑9 hours of dark, quiet rest. If you toss and turn, keep the room cool, avoid screens an hour before bed, and consider a lightweight pillow that supports your neck without forcing your head forward.
Food can be a hidden pain driver. Processed snacks high in sugar and bad fats can inflame nerves. Swap them for omega‑3 rich foods like salmon, walnuts, or flaxseed. Add colorful veggies and fruits for antioxidants that calm inflammation. Staying hydrated helps joints glide smoothly, so sip water throughout the day.
Medications and therapies you can consider
Over‑the‑counter options such as ibuprofen or naproxen can relieve mild‑to‑moderate aches, but they’re not for everyone. If you have stomach issues or take blood thinners, talk to a pharmacist before reaching for them. Prescription drugs like low‑dose antidepressants or anti‑seizure meds often help nerve‑related pain, but they need a doctor’s green light.
Physical therapy isn’t just for athletes. A skilled therapist can teach you movement patterns that protect sore spots and strengthen supporting muscles. Even a few sessions can give you a home‑exercise plan that reduces flare‑ups.
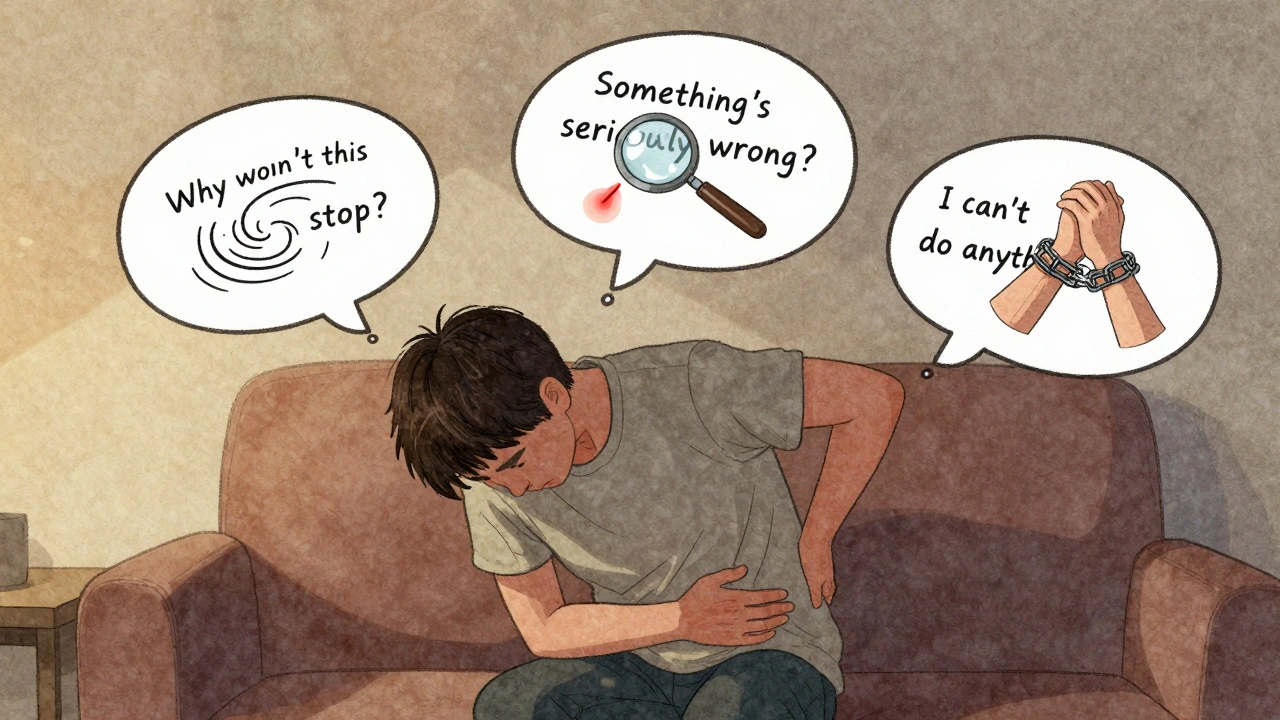
Mind‑body approaches are underrated. Cognitive‑behavioral therapy (CBT) teaches you to re‑frame pain thoughts, which can lower the perceived intensity. Simple mindfulness breathing or guided meditation for ten minutes a day also lowers stress hormones that make pain worse.
When pain spikes, heat or cold packs can offer quick relief. Heat relaxes tight muscles, while ice numbs sharp, inflamed areas. Switch between them depending on what feels better for the specific ache.
Finally, keep a pain journal. Jot down when the pain hits, what you ate, your activity level, and any meds you took. Patterns will emerge, and you can share this info with your doctor to fine‑tune treatment.
Managing chronic pain isn’t a one‑size‑fits‑all plan, but mixing a few daily habits with the right meds and therapies can dramatically improve your quality of life. Start with one small habit today, track what works, and build from there—you deserve relief.