When your pain feels like it’s taking over your whole life-when every twinge makes you think, “This is never going to get better,” or “I can’t handle this anymore”-you’re not just feeling physical discomfort. You’re caught in a mental loop called pain catastrophizing. It’s not weakness. It’s not laziness. It’s a real, measurable psychological pattern that makes pain feel worse, last longer, and steal more from your life than it should.
Research shows pain catastrophizing is one of the strongest predictors of poor outcomes in chronic pain. People who catastrophize report higher pain intensity, more disability, longer recovery times, and even higher risk of depression and anxiety. But here’s the good news: it’s not permanent. You can change it. And one of the most proven ways to do that is through Cognitive Behavioral Therapy, or CBT.
What Exactly Is Pain Catastrophizing?
Pain catastrophizing isn’t just being negative. It’s a specific set of thoughts that kick in when you’re in pain-or even when you think pain might come back. The Pain Catastrophizing Scale (PCS), developed in the 1990s and still the gold standard for measuring it, breaks it down into three parts:
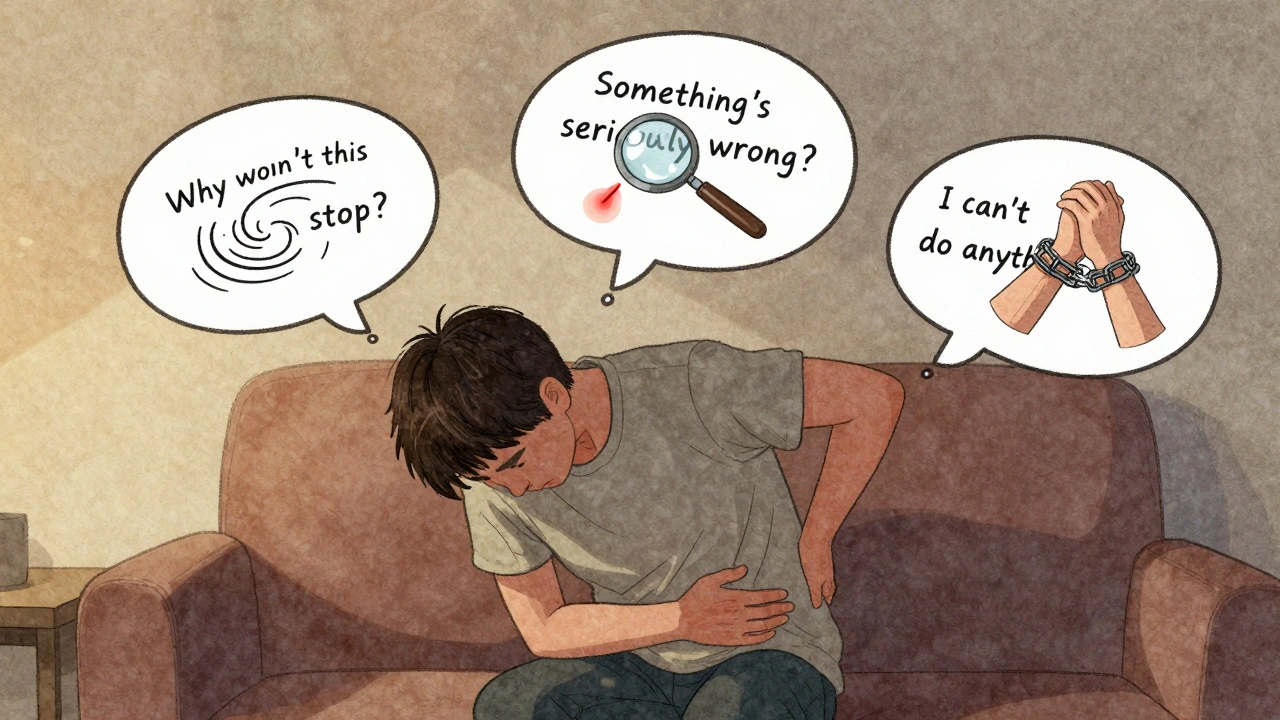
- Rumination: You can’t stop thinking about the pain. It replays in your head like a broken record: “Why won’t this stop? What if it gets worse?”
- Magnification: You blow the threat out of proportion. A small ache becomes “This is a sign something’s seriously wrong.”
- Helplessness: You feel like you have no control. “There’s nothing I can do. I’m trapped.”
These thoughts don’t just live in your mind-they physically change how your brain processes pain. Brain scans show that when someone catastrophizes, areas linked to emotion and threat detection light up more intensely. That means your brain doesn’t just register the pain signal-it amplifies it. The result? More suffering, even if the physical injury hasn’t changed.
How CBT Breaks the Cycle
CBT doesn’t tell you to “think positive.” It doesn’t ignore your pain. Instead, it helps you notice the difference between what’s actually happening in your body and what your mind is telling you about it.
Think of it like this: Your body sends a signal-say, a dull ache in your lower back. Your brain, trained by past experiences and fear, adds its own story: “This is the start of a flare-up. I’m going to be stuck in bed for days. I’ll lose my job. I’ll never be myself again.” That story creates fear, tension, and avoidance. And guess what? Avoiding movement makes your muscles tighter, your nervous system more sensitive, and your pain worse.
CBT interrupts that loop. It teaches you to step back and ask: “Is this thought based on facts-or fear?”
Three CBT Tools That Actually Work
1. Self-Monitoring: Track the Pattern
Before you can change a thought, you need to see it clearly. Start keeping a simple pain log. Each day, write down:
- What happened right before the pain spiked?
- What thoughts ran through your head?
- How did you feel emotionally?
- What did you do in response?
Example:
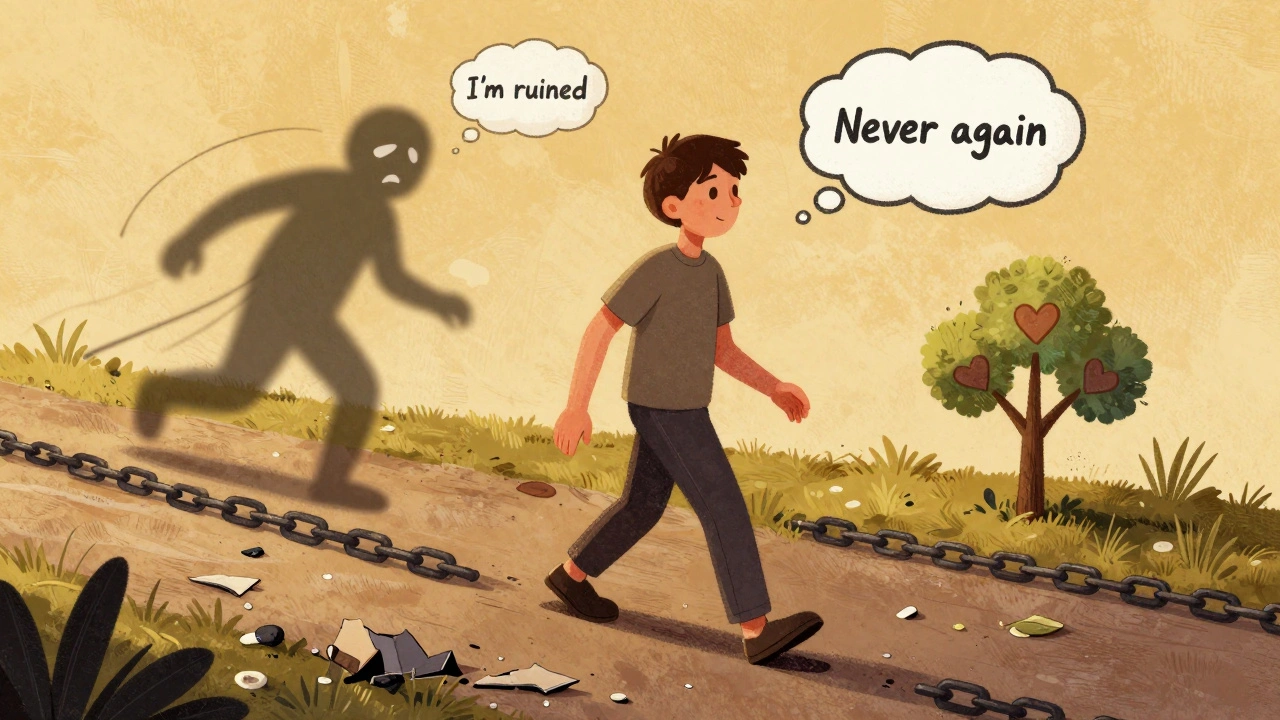
“Tried to carry groceries. Pain shot up to 7/10. Thought: ‘I’m ruined. I’ll never be able to do this again.’ Felt panic. Sat down and didn’t move for an hour.”
After a week, you’ll start seeing patterns. Maybe you catastrophize most after bad nights’ sleep. Or maybe it happens every time you hear a certain sound-like a door slamming-that reminds you of a past injury. Awareness is the first step to control.
2. Cognitive Restructuring: Challenge the Story
Once you spot a catastrophic thought, don’t fight it. Don’t try to replace it with a happy one. Just question it.
Ask yourself:
- What’s the evidence this thought is true?
- What’s the evidence it’s not true?
- What’s the worst that could realistically happen?
- What’s a more balanced way to see this?
Take the thought: “This pain means I’m getting worse.”
Challenge it:
- Evidence it’s true: “I’ve had pain for months.”
- Evidence it’s not: “My pain has gone up and down. Last month, I had a week where it was barely there.”
- Realistic worst case: “I might have a bad day. But I’ve had bad days before and recovered.”
- Balanced thought: “This pain is uncomfortable, but it doesn’t mean I’m deteriorating. It’s just a flare.”
It’s not about pretending everything’s fine. It’s about replacing panic with perspective.
3. Behavioral Activation: Move Even When It’s Hard
When you’re in pain, your brain tells you to rest. But rest becomes avoidance. And avoidance feeds fear. CBT encourages gentle, consistent movement-not to “fix” the pain, but to prove to your brain that movement won’t destroy you.
Start small. Pick one activity you’ve avoided because you feared it would make things worse. Maybe it’s walking to the mailbox. Or standing up to make tea. Do it anyway-even if your pain goes up a point or two. Then record what happened afterward.
Most people find: “The pain went up, but it didn’t spiral. I didn’t collapse. I recovered within a few hours.” That’s the data your brain needs to unlearn the fear.

Who Benefits Most From CBT for Pain Catastrophizing?
Studies show CBT works best for people who:
- Have chronic pain that’s been going on for more than three months
- Feel stuck in a cycle of worry and inactivity
- Have tried medications or physical therapy but still feel emotionally overwhelmed
- Are willing to do a little work outside of sessions
It’s not a magic cure. It’s a skill. And like any skill, it takes practice. Most people start noticing changes after 4-6 weeks. By week 10-12, many report significant drops in both catastrophizing scores and pain intensity.
One case from the Journal of Pain Research followed a 45-year-old woman with fibromyalgia. Her PCS score (a measure of catastrophizing) dropped from 42 to 18 after 12 weeks of CBT. Her pain intensity fell by half. She went back to part-time work.
What Doesn’t Work
Some people try to use CBT when their pain is at its worst-like when it’s an 8 or 9 out of 10. That’s when the mental load is too high. You can’t restructure thoughts when your brain is in survival mode.
That’s why timing matters. Start CBT during a quieter phase. Use it to build resilience so you’re better prepared when flare-ups come.
Also, CBT isn’t a substitute for treating depression, anxiety, or PTSD-if those are present, they need their own care. Pain catastrophizing often rides on top of other mental health issues. Addressing them together gives the best results.
Getting Started: Where to Find Help
You don’t need to go it alone. Many hospitals, pain clinics, and VA centers now include CBT as part of standard pain care. Since 2020, the U.S. Veterans Health Administration has required all chronic pain patients to be screened for catastrophizing-and offered CBT if needed.
If you’re not near a specialized clinic, look for:
- Psychologists licensed in pain management
- Online CBT programs like Curable or PainScale (used by over 450,000 people as of early 2024)
- Group programs offered through community health centers
Some insurance plans cover CBT for chronic pain. Ask your provider. If cost is a barrier, many universities with psychology programs offer low-cost services through training clinics.
The Bigger Picture
Pain catastrophizing isn’t your fault. It’s a survival mechanism gone wrong. Your brain was trying to protect you by warning you to stop, rest, and avoid danger. But in chronic pain, that system gets stuck.
CBT doesn’t erase pain. But it gives you back your power. You stop being a victim of your thoughts. You become the observer. The questioner. The one who chooses how to respond.
By 2025, 75% of pain clinics in the U.S. will routinely screen for catastrophizing. That’s because we now know: treating the mind isn’t optional. It’s essential.
You don’t have to live in fear of your own pain. The tools are here. The science is clear. And you’re already taking the first step-by reading this.
Is pain catastrophizing the same as being negative or weak?
No. Pain catastrophizing is a specific psychological pattern, not a personality flaw. It’s a learned response that your brain uses to cope with ongoing threat. Many strong, resilient people experience it. The fact that you’re asking this question means you’re already moving toward change.
How long does CBT take to work for pain catastrophizing?
Most people start noticing shifts in their thinking after 3-4 weeks. Significant reductions in catastrophizing and pain distress typically show up between 8 and 12 weeks of consistent practice. Like learning to ride a bike, it takes time to build the skill, but once it’s there, it lasts.
Can I do CBT on my own, or do I need a therapist?
You can start with self-guided tools like apps (Curable, PainScale) or workbooks. Many people benefit from this. But working with a trained therapist-especially one experienced in chronic pain-doubles your chances of success. They help you spot blind spots, adjust techniques, and stay on track when motivation dips.
Does CBT work if I’m still in a lot of pain?
Yes-but it’s easier when your pain is lower. CBT helps you build tools to handle pain better, not eliminate it. Think of it like learning to swim: you don’t wait until the ocean is calm to practice. You start in the shallow end. Use CBT during quieter days to build strength, so when pain flares, you’re better equipped.
What if I tried CBT before and it didn’t work?
Many people quit too early. CBT isn’t a quick fix. It’s a mental rewiring process. If your first attempt failed, ask yourself: Did you give it 8-12 weeks? Were you tracking your thoughts? Did you have support? Sometimes, switching therapists or trying a different approach (like combining CBT with mindfulness) makes all the difference.
Next Steps If You’re Ready
Start today. Grab a notebook. Write down one catastrophic thought you’ve had this week. Then write down one fact that contradicts it. That’s it. You’ve already begun.
CBT doesn’t promise a pain-free life. But it does promise a life where pain doesn’t own your mind. And that’s worth more than you think.

Jack Appleby
Let’s be clear: pain catastrophizing isn’t some new-age buzzword-it’s a neurocognitive distortion with fMRI validation dating back to Sullivan’s 1995 PCS scale. The fact that you’re still framing CBT as a ‘tool’ rather than a neuroplasticity-driven recalibration of the anterior cingulate and insular cortex suggests a fundamental misunderstanding of the mechanism. This isn’t ‘thinking positively.’ It’s top-down modulation of nociceptive processing via prefrontal inhibition. If you’re not tracking cortical activation patterns alongside your pain logs, you’re just journaling.
Frank Nouwens
Thank you for this thoughtful and well-researched piece. I’ve worked with chronic pain patients for over two decades, and I can say with confidence that the CBT framework you’ve outlined is among the most humane and evidence-based approaches available. Many of my clients initially resist the idea that their thoughts affect their pain-but once they see the pattern in their logs, the shift is often profound. Small steps, indeed.
Jean Claude de La Ronde
so like... we're supposed to 'restructure' our thoughts so our brain stops screaming 'YOU'RE DYING' every time we sneeze? cool. next you'll tell me my spine is just being dramatic and needs a pep talk. also, who wrote this? a grad student who got paid in coffee and existential dread?
Mia Kingsley
OMG I HATE THIS SO MUCH. CBT IS JUST A WAY FOR DOCTORS TO SAY 'IT'S ALL IN YOUR HEAD' AND NOT PRESCRIBE MORE OPIATES. I'VE BEEN IN PAIN FOR 8 YEARS AND NO ONE LISTENS. NOW I'M SUPPOSED TO JUST 'THINK DIFFERENTLY'? WHAT ABOUT MY ACTUAL SPINAL STENOSIS? THIS ARTICLE IS SO TOXIC I'M CRYING. WHY DO PEOPLE THINK PAIN IS A CHOICE??
Katherine Liu-Bevan
Thank you for sharing this. I’ve seen firsthand how catastrophizing traps people in a cycle of fear and immobility. The key isn’t to dismiss the pain-it’s to separate the sensation from the story. One client, a former dancer with degenerative disc disease, started with a PCS score of 45. After 10 weeks of self-monitoring and graded exposure, she returned to yoga. Not because the pain vanished, but because she no longer believed it meant disaster. The data doesn’t lie: cognitive flexibility reduces suffering. Start small. Be patient. You’re not broken.
Aman deep
Bro, this hit different. I got neuropathic pain from a work injury, and I used to think every twinge meant I was ruined. Started writing down my thoughts like you said-turned out I was always assuming the worst because my dad used to scream 'you'll never walk right again' after my first surgery. Realized I was replaying his voice, not my reality. Took me months, but now when pain spikes, I say: 'this is old noise, not new danger.' Not magic. Just truth.
Sylvia Frenzel
This is why America is falling apart. We’re turning real medical conditions into therapy exercises. If your spine is damaged, get surgery. If you’re in pain, take the pill. Stop making people feel guilty for needing help. This isn’t empowerment-it’s gaslighting disguised as science.
Doris Lee
You’re not alone. I’ve been here too. Start with one tiny thing today-maybe just standing up to stretch. You don’t have to believe it’ll work. Just do it. And if it hurts? That’s okay. You’re still moving. That’s the win.