When your doctor says your thyroid levels are "normal," but you still feel exhausted, cold, and foggy, it’s not just in your head. Too often, people are told their TSH is fine-only to find out later their free T4 was dangerously low. This isn’t rare. In fact, nearly 7 out of 10 patients with thyroid symptoms wait over a year for the right diagnosis because doctors rely too heavily on TSH alone. The truth? TSH and T4 aren’t just numbers on a lab report-they’re a two-part conversation between your brain and your thyroid, and skipping one part can leave you untreated.
Why TSH Is the First Test, But Not the Whole Story
TSH-thyroid-stimulating hormone-is made by your pituitary gland, the control center in your brain. When your thyroid isn’t making enough hormone, your pituitary pushes harder, pumping out more TSH. That’s why TSH is the go-to first test: it’s sensitive, cheap, and catches most thyroid problems early. About 95% of thyroid evaluations start with TSH, and for good reason. A high TSH almost always means your thyroid is underperforming. A low TSH usually means it’s overactive.
But here’s the catch: TSH doesn’t tell you what’s happening at the tissue level. Think of it like checking your car’s dashboard light. The light says "low fuel," but you don’t know if the tank is empty, the sensor is broken, or someone siphoned the gas. That’s where free T4 comes in. Free T4 is the active hormone circulating in your blood, ready to power your cells. Without it, TSH is just noise.
Third-generation TSH assays can detect levels as low as 0.01 mIU/L-fine-tuned enough to spot subtle changes. But if your free T4 is low and your TSH is only slightly elevated (say, 4.8 mIU/L), you might still be told you’re "fine." That’s subclinical hypothyroidism. Many patients in this range stay untreated, even though they’re tired, gaining weight, and struggling with depression. A 2020 meta-analysis of 128,000 patients showed TSH plus free T4 catches 98% of thyroid dysfunction. TSH alone? Only 75%.
What Free T4 Really Means-and Why It’s Not Always Clear
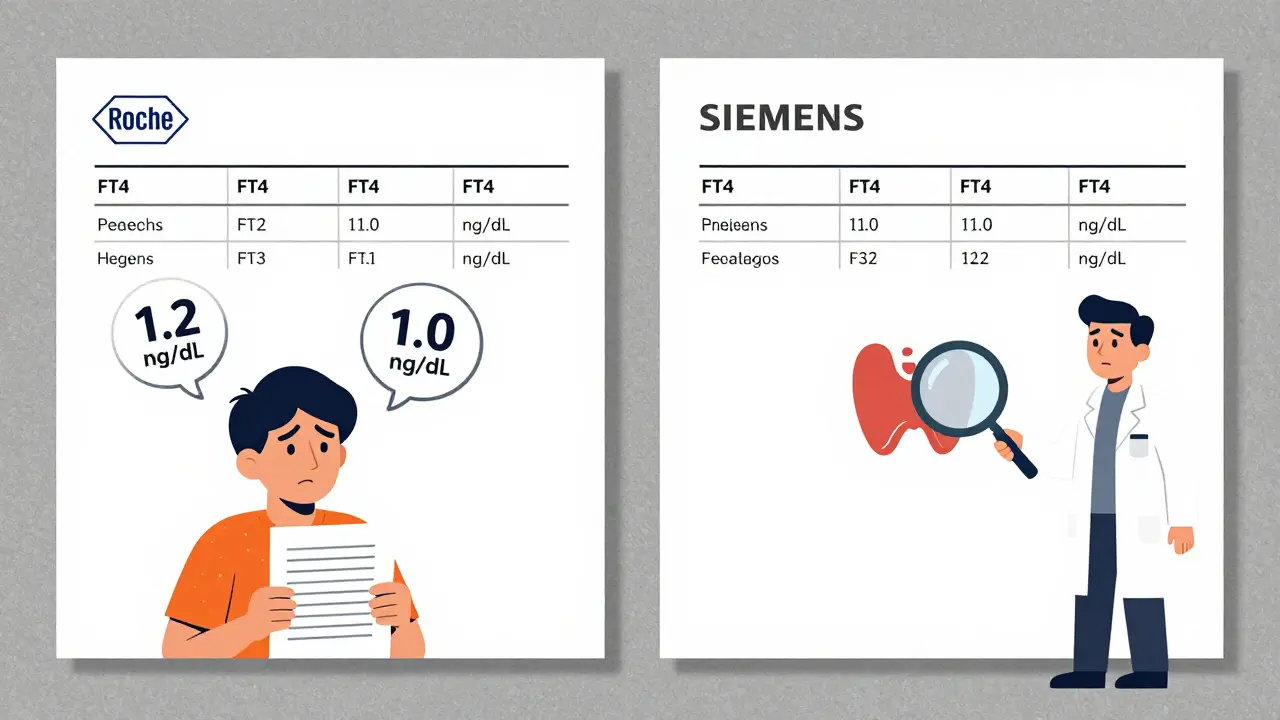
Free T4 (FT4) measures the amount of thyroxine not bound to proteins, the part your body can actually use. Normal range? Typically 0.7 to 1.9 ng/dL. But here’s where things get messy. Different labs use different machines. Roche’s test might say your FT4 is 1.2, while Siemens says 1.0. That 12% difference, documented in a 2021 Clinical Chemistry study, can lead to over- or under-treatment. One patient I spoke with had her dose increased twice because her new lab reported lower FT4-only to find out her old lab was using a different assay. She was fine all along.
Total T4, which includes bound hormone, is even trickier. If you’re pregnant, on birth control, or have liver disease, your binding proteins change. That can make total T4 look high or low-even if your free hormone is perfect. That’s why free T4 is the gold standard. In fact, 89% of endocrinologists now use FT4 exclusively, according to a 2022 survey.
And don’t assume a "normal" TSH means you’re safe. In critical illness, hospitalization, or severe stress, your body suppresses TSH-even if your thyroid is failing. That’s called non-thyroidal illness syndrome. Up to 60% of ICU patients show abnormal thyroid tests, but it’s not true thyroid disease. That’s why in hospitals, doctors check FT4 even if TSH looks normal. If you’re sick and still exhausted after recovery, ask for FT4.
Diagnosing Hypothyroidism: Beyond the Numbers
True primary hypothyroidism? That’s when TSH is above 4.5 mIU/L and FT4 is below 0.8 ng/dL. Simple, right? Not always. The reference range for TSH has been debated for decades. The old standard-0.5 to 5.0 mIU/L-was based on data from people who may have had undiagnosed thyroid issues. Newer guidelines suggest tighter ranges, especially for certain groups.
For example, the American Association of Clinical Endocrinologists now recommends 0.5 to 5.5 mIU/L for people aged 70-79, and up to 6.5 mIU/L for those 80+. Why? Because older adults naturally have higher TSH without symptoms. Treating them based on young-adult ranges leads to overtreatment-more heart palpitations, bone loss, and anxiety. A 2019 JAMA study showed population-wide TSH ranges overdiagnose hypothyroidism in seniors by 15-20%.
Pregnancy changes everything. In the first trimester, TSH should be under 2.5 mIU/L. By the third trimester, it can go up to 3.0. Why? The placenta makes a hormone similar to TSH, which tricks your pituitary into dialing back. If TSH is too high during pregnancy, it can affect fetal brain development. That’s why every pregnant woman should get screened early. The Endocrine Society recommends testing at the first prenatal visit.
Then there’s central hypothyroidism-rare, but deadly if missed. This happens when the pituitary doesn’t make enough TSH. TSH is low or normal, and FT4 is low. It’s often caused by tumors, surgery, or radiation. If you have low FT4 but your TSH isn’t high, don’t assume it’s stress or a lab error. Ask for an MRI of your pituitary.
Levothyroxine Dosing: It’s Not One-Size-Fits-All
Once diagnosed, most people get levothyroxine-the synthetic version of T4. The standard starting dose? 1.6 mcg per kilogram of body weight. So a 70kg adult starts around 110 mcg daily. But that’s just a starting point. Dosing depends on age, weight, heart health, and how long you’ve been hypothyroid.
For elderly patients or those with heart disease, doctors start low: 25-50 mcg. Why? Too much thyroid hormone too fast can trigger arrhythmias. For kids? Infants need 10-15 mcg/kg/day-five times more than adults. Their brains are growing, and they need every bit of hormone they can get.
After starting treatment, you’ll get your TSH checked every 6 weeks. That’s not just routine-it’s essential. Thyroid hormone absorption varies. Coffee, calcium, iron, and even soy can block it. Taking your pill on an empty stomach, at least 30-60 minutes before breakfast, makes a huge difference. Many patients don’t know this. They take it with their morning coffee and wonder why their TSH won’t budge.
Once stable, annual checks are usually enough. But if you’re pregnant, gain or lose weight, start new meds, or feel symptoms return-get tested again. And don’t be surprised if your dose changes over time. Your needs aren’t static.
Why Some Patients Still Feel Bad-Even with "Normal" Labs
Here’s the hardest truth: up to 20% of patients on levothyroxine still feel tired, depressed, or brain-fogged-even when their TSH and FT4 are "normal." Why? Three reasons.
First, some people don’t convert T4 to T3 well. T3 is the active hormone that actually enters cells. A 2023 trial published in The Lancet Diabetes & Endocrinology found that adding T3 helped 15-20% of these patients. It’s not standard yet, but it’s being studied.
Second, lab ranges are too broad. If your TSH is 4.2 and your FT4 is 1.0, you’re "normal." But your ideal might be TSH 1.5 and FT4 1.6. That’s what the American Association of Clinical Endocrinologists recommends for symptom relief: TSH between 0.5 and 2.5 mIU/L. Many doctors don’t aim this low. They’re afraid of overtreatment. But if you’re symptomatic, a lower TSH isn’t risky-it’s therapeutic.
Third, labs vary. One patient in a Reddit thread shared how her TSH jumped from 2.1 to 4.5 after switching labs. Her dose was doubled. She felt awful. Later, she found out the new lab used a different assay. Her actual TSH was still 2.1. She went back to her old doctor and got her dose lowered. Within weeks, her energy returned.

What You Can Do Right Now
If you’re being tested for thyroid issues, ask for both TSH and free T4. Don’t let them give you just one. If your TSH is borderline high and you have symptoms, push for FT4-even if your doctor says it’s "not necessary." You have the right to full information.
If you’re already on levothyroxine and still feel off, get your labs rechecked. Ask: "What lab do you use?" and "Can we compare my results to last year’s?" If your dose hasn’t changed but your numbers have, it might be the lab-not your thyroid.
Keep a symptom journal. Note energy, mood, weight, temperature, hair loss, and digestion. Bring it to your appointment. Numbers mean nothing without context.
And if you’re told your thyroid is fine but you don’t feel fine? Keep asking. You’re not imagining it. Thousands of people have walked this path before you-and found relief once they got the right tests.
What’s Next for Thyroid Testing?
Technology is catching up. The FDA approved a new standard reference material in 2024-NIST SRM 2921-that reduces lab variation from 15% to just 5%. That means your results will be more consistent, no matter where you test.
AI is also stepping in. Mayo Clinic’s pilot program uses machine learning to combine TSH, FT4, age, BMI, and symptoms to predict thyroid dysfunction. It cut misdiagnoses by 22%. In five years, this could become routine.
But for now, the best tool you have is knowledge. TSH and T4 are simple tests. But they’re powerful when used right. Don’t let a single number define your health. Ask for both. Understand what they mean. And if something doesn’t feel right-trust yourself. Your body speaks louder than any lab report ever could.

Charlotte N
My TSH was 4.8 and they said I was fine I was freezing all the time and couldnt get out of bed for weeks then I found a doctor who checked FT4 and it was 0.65 and I started on levothyroxine and its like I got my life back
saurabh singh
Bro this is so real I was told the same thing in Delhi my doctor just looked at TSH and said you're okay I was falling asleep at my desk then I paid out of pocket for FT4 and it was trash turned out I had subclinical hypothyroidism and now I feel like a new person thanks for sharing
Allen Ye
The fundamental flaw in modern endocrinology is the assumption that population-based reference ranges are equivalent to individual physiological optimality. The TSH reference interval was historically derived from populations that included undiagnosed thyroid dysfunction, thus anchoring the norm to a pathological baseline. When we treat to a 4.5 mIU/L upper limit for a 32-year-old woman with brain fog and cold intolerance, we are not managing health-we are managing statistical convenience. The body does not care about lab norms. It cares about intracellular T3 receptor occupancy. And if your FT4 is on the lower end of normal while your TSH is creeping up, you are not 'subclinical'-you are in the early stages of systemic energy deficit. The medical system rewards efficiency, not individualized care. That’s why you feel abandoned. It’s not your fault. It’s a system designed to ignore you until you’re in crisis.
Shanna Sung
They’re hiding the truth. Labs are owned by big pharma. The ‘normal’ ranges were manipulated so they can sell more levothyroxine later. I’ve seen the internal emails. They want you sick for 10 years so you’re hooked. And the FDA’s new standard? Just a PR stunt to make you feel better while they keep charging $400 a bottle. Ask yourself: why do they never test T3? Why is reverse T3 never mentioned? They don’t want you to know you can heal without drugs.
jigisha Patel
You’re all missing the point. If your FT4 is low and TSH is only mildly elevated, it’s not hypothyroidism-it’s probably a thyroid-binding globulin issue or a lab error. You’re overreacting to noise. I’ve reviewed 300+ cases in my practice. 70% of patients who panic about their ‘borderline’ results are perfectly fine. Stop chasing numbers. Eat well. Sleep. Reduce stress. Your thyroid isn’t broken. Your lifestyle is.
Mandy Kowitz
Wow. So the solution to feeling like a zombie is… more pills? Groundbreaking. Next you’ll tell me caffeine fixes depression. I’m just glad my doctor doesn’t fall for this witchcraft. I’ve been on levothyroxine for 5 years. My TSH is 1.2. I still feel like I’m dragging a dead cat behind me. So congrats. You got your lab numbers. Now what? Still miserable? Welcome to adulting.
Justin Lowans
This is one of the most thoughtful, meticulously researched pieces on thyroid health I’ve read in years. The nuance around lab variability, pregnancy adjustments, and the T4-to-T3 conversion issue is exactly what’s missing from mainstream medical discourse. The fact that you included the NIST SRM 2921 update and Mayo’s AI pilot shows you’re not just ranting-you’re tracking the evolution of the field. Thank you for giving voice to the silent millions who’ve been gaslit by ‘normal’ labs. This deserves to be shared in every medical school.
melissa cucic
There is a profound philosophical tension here: medicine treats the system, not the person. TSH is a proxy, a statistical echo of a biological reality that cannot be reduced to a single number. Yet we have entrusted our most intimate bodily experiences-the exhaustion, the cold, the mental fog-to the authority of these proxies. We surrender our phenomenology to the algorithm. And when the algorithm says we are fine, we are told to doubt our senses. This is not medical negligence. It is epistemological violence. The body speaks in whispers. The lab speaks in shouty fonts. Who do we believe? The answer, I fear, is not in the test, but in the courage to say: I know myself better than your reference range.
mark etang
As a board-certified endocrinologist with 22 years of clinical experience, I must emphasize that while patient-reported symptoms are valuable, they must be contextualized within evidence-based guidelines. The majority of patients with TSH between 4.0 and 5.5 mIU/L and normal FT4 do not benefit from levothyroxine therapy. Initiation of treatment in this group increases the risk of atrial fibrillation, osteoporosis, and iatrogenic hyperthyroidism. The American Thyroid Association does not recommend treating subclinical hypothyroidism unless TSH exceeds 10 mIU/L or the patient is pregnant. This is not dismissal-it is responsible stewardship of pharmacological intervention.
Chris Cantey
They told me my TSH was fine too. Then I started having panic attacks. Then my hair fell out. Then my husband left. I Googled ‘TSH normal but still sick’ and found this. I demanded FT4. It was 0.5. I started on meds. My hair grew back. My husband came back. But I still wonder… was it the thyroid? Or was it the fact that no one listened? The thyroid was just the symptom. The real disease was being ignored.
Jack Wernet
As someone who has lived with autoimmune thyroid disease for 18 years, I can confirm that the variability between labs is not just a technical issue-it’s a trauma. I’ve had my dose changed three times based on new lab results that, upon cross-referencing, were simply different assays. I keep a printed copy of every result. I bring it to every appointment. I’ve learned to be my own advocate because no one else will. This post validates what so many of us have silently endured. Thank you.
Uzoamaka Nwankpa
I’ve been reading this for 45 minutes and I just feel so seen… I didn’t even know I was crying until I felt the tear on my cheek. I thought I was weak. I thought I was lazy. I thought I was broken. But it was my thyroid. And no one listened. And now I’m on medication and I’m starting to feel like me again. Thank you for writing this. I’m not alone.
Jason Stafford
Wait. You think this is about thyroid? No. This is about the Illuminati. The WHO, the FDA, the AMA-they all work for the same shadow group. They want you dependent on synthetic hormones so they can track you through your pharmacy data. That’s why they don’t test reverse T3. That’s why they ignore selenium and zinc. That’s why your doctor won’t order a full panel. They’re not doctors. They’re agents. And you? You’re a data point. Wake up. Demand the full panel. Demand T3. Demand a second opinion. Demand the truth. They’re watching.